
Contributions
Abstract: PB1673
Type: Publication Only
Session title: Myeloma and other monoclonal gammopathies - Clinical
Background
The introduction of new agents and classes of therapy has improved outcomes in patients with multiple myeloma (MM). However, there is limited understanding of the variations in use of new therapies across different geographical regions and the extent to which these variations translate into improved outcomes.
Aims
To perform a systematic literature review (SLR) to investigate trends in MM treatment patterns and clinical outcomes reported in published real-world studies.
Methods
Searches were performed in PubMed and EMBASE from January 2010 to November 2020 to identify English-language publications reporting the efficacy and safety of therapies for patients with newly diagnosed MM (NDMM) and relapsed or refractory MM (RRMM) in any geographical region. Relevant conferences in 2019 and 2020 were also searched. The citations were systematically screened in 3 stages following predefined eligibility criteria (PICOs). Data were analysed in MS excel and the relevant data extracted for further interpretation.
Results
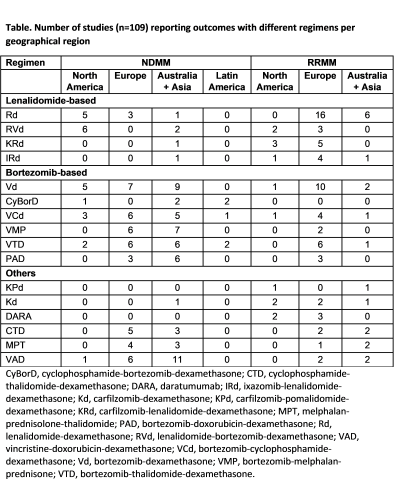
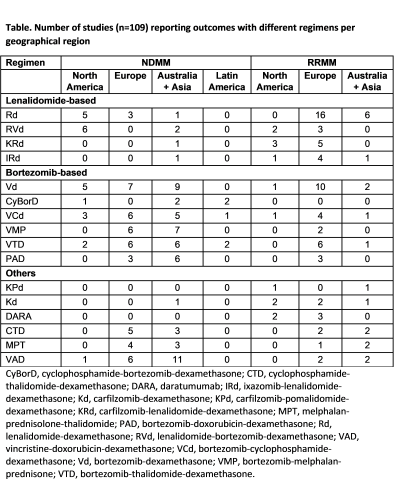
A total of 472 publications were identified; 60% were published in 2016 or later. Most reported findings for studies conducted in Europe (n=180 [38%]), North America (n=98 [21%]), or Asia (n=171 [36%]). Almost half (n=222 [47%]) involved patients with RRMM, 41% (n=195) included patients with NDMM and 12% (n=55) had a mix of MM populations. A total of 149 publications described multicentre/claims database/registry studies involving >50 patients. Of these, 28 reported median OS and 23 reported median PFS data. Median OS was 5.2–60.0 months in patients with NDMM and 5.4–41.9 months in patients with RRMM. Median PFS was 10.3–33.6 months in patients with NDMM and 4.9–27.6 months in patients with RRMM. Differences in the most commonly cited regimens were noted between geographical regions (Table). In studies reporting outcomes in patients with NDMM, bortezomib-based regimens predominated in Europe and Asia, whereas in US studies, lenalidomide + dexamethasone (Rd)–based regimens and bortezomib-based regimens were equally described. The most commonly described bortezomib-based regimens in Europe and Asia were bortezomib + dexamethasone (Vd), VCd, VMP, and VTD. In studies reporting outcomes in patients receiving treatment for RRMM, Rd and Rd-based triplets (including RVd, KRd, and IRd) were the most commonly used regimens across the 3 regions. Bortezomib-based regimens described in >4 European studies included Vd, VCd, and VTD. Few US or Asian studies described bortezomib-based regimens. Differences in efficacy outcomes according to geographical regions will be presented.
Conclusion
The findings from the SLR indicate that, over the last 10–15 years, there have been differences in the reported use of the new therapies and regimens in different geographical regions, particularly between North America vs Europe and Asia. Reported survival outcomes differ widely between different studies, possibly reflecting differences in regimens used and patient management. Understanding these differences in real-world clinical practice and their outcomes will help inform clinicians of the optimal use of available treatments, identify unmet needs, and help further improve long-term outcomes for patients.
Keyword(s): Clinical outcome, Multiple myeloma, Systematic review, Treatment
Abstract: PB1673
Type: Publication Only
Session title: Myeloma and other monoclonal gammopathies - Clinical
Background
The introduction of new agents and classes of therapy has improved outcomes in patients with multiple myeloma (MM). However, there is limited understanding of the variations in use of new therapies across different geographical regions and the extent to which these variations translate into improved outcomes.
Aims
To perform a systematic literature review (SLR) to investigate trends in MM treatment patterns and clinical outcomes reported in published real-world studies.
Methods
Searches were performed in PubMed and EMBASE from January 2010 to November 2020 to identify English-language publications reporting the efficacy and safety of therapies for patients with newly diagnosed MM (NDMM) and relapsed or refractory MM (RRMM) in any geographical region. Relevant conferences in 2019 and 2020 were also searched. The citations were systematically screened in 3 stages following predefined eligibility criteria (PICOs). Data were analysed in MS excel and the relevant data extracted for further interpretation.
Results
A total of 472 publications were identified; 60% were published in 2016 or later. Most reported findings for studies conducted in Europe (n=180 [38%]), North America (n=98 [21%]), or Asia (n=171 [36%]). Almost half (n=222 [47%]) involved patients with RRMM, 41% (n=195) included patients with NDMM and 12% (n=55) had a mix of MM populations. A total of 149 publications described multicentre/claims database/registry studies involving >50 patients. Of these, 28 reported median OS and 23 reported median PFS data. Median OS was 5.2–60.0 months in patients with NDMM and 5.4–41.9 months in patients with RRMM. Median PFS was 10.3–33.6 months in patients with NDMM and 4.9–27.6 months in patients with RRMM. Differences in the most commonly cited regimens were noted between geographical regions (Table). In studies reporting outcomes in patients with NDMM, bortezomib-based regimens predominated in Europe and Asia, whereas in US studies, lenalidomide + dexamethasone (Rd)–based regimens and bortezomib-based regimens were equally described. The most commonly described bortezomib-based regimens in Europe and Asia were bortezomib + dexamethasone (Vd), VCd, VMP, and VTD. In studies reporting outcomes in patients receiving treatment for RRMM, Rd and Rd-based triplets (including RVd, KRd, and IRd) were the most commonly used regimens across the 3 regions. Bortezomib-based regimens described in >4 European studies included Vd, VCd, and VTD. Few US or Asian studies described bortezomib-based regimens. Differences in efficacy outcomes according to geographical regions will be presented.
Conclusion
The findings from the SLR indicate that, over the last 10–15 years, there have been differences in the reported use of the new therapies and regimens in different geographical regions, particularly between North America vs Europe and Asia. Reported survival outcomes differ widely between different studies, possibly reflecting differences in regimens used and patient management. Understanding these differences in real-world clinical practice and their outcomes will help inform clinicians of the optimal use of available treatments, identify unmet needs, and help further improve long-term outcomes for patients.
Keyword(s): Clinical outcome, Multiple myeloma, Systematic review, Treatment


