
Contributions
Abstract: PB1671
Type: Publication Only
Session title: Myeloma and other monoclonal gammopathies - Clinical
Background
Cross-sectional MRI imaging has a growing importance in the classification of plasma cell dyscrasias, and in the definition of multiple myeloma (MM) response or progression (Dimopoulos 2015, Chantry 2017). High sensitivity of a diffusion-weighted whole body MRI (DW-WBMRI) in the early detection of bone marrow changes has been acknowledged in the revised IMWG diagnostic criteria (Rajkumar et al, 2014). A multidisciplinary imaging and haematologist expert panel has supported the measurement of cell density using an apparent diffusion coefficient (ADC) for the early diagnosis of changes in bone marrow infiltration and myeloma focal lesions (Messiou 2019). Recommendations for myeloma diagnosis and response assessment has been published (MYRADS) recently. We used data from a prospective plasma cell dyscrasias imaging study (NCT03951220) to validate these recommendations.
Aims
This prospective imaging study used a DW-MRI protocol to quantify longitudinal changes in tumour burden and bone disease. To improve sensitivity of bone marrow lesion identification healthy volunteers (HV) were also recruited. One of the study aims is to validate MYRADS protocol recommendations.
Methods
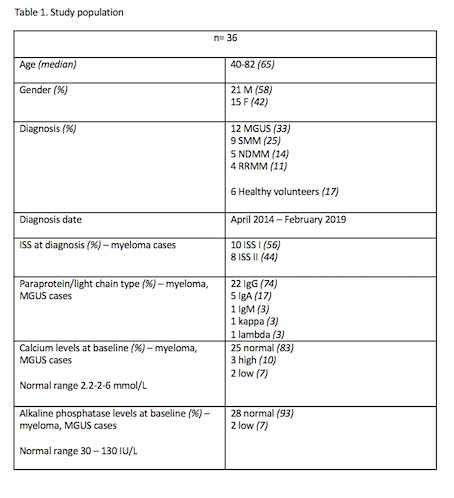
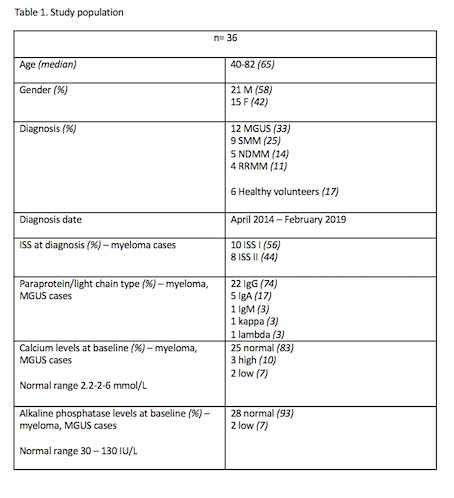
To validate the recommendations in the MYRADS protocol we took an unselected population of 18 MM pts, 12 MGUS pts and 6 HVs recruited between April 2018 and January 2019. See Table 1 for participants’ characteristics. After enrolment patients had a DW-WBMRI abbreviated protocol on the 3T Avanto MRI scanner (Siemens, Germany). In 18 participants with MM and MGUS the scan was repeated after 6 months using the same protocol. Qualitative assessment of bone marrow changes were made using the MYRADS recommendations. In each positive scan (Myeloma patients) we used the changes in ADC value (quantitative) of a single lytic lesion (MYRADS response assessment categories) and matched them with the serological parameters of disease.
Results
All 36 participants safely completed the protocol at baseline. Ten scans (28%) were positive for vertebral fractures (1 to 8 vertebral bodies involved); pathological fractures were associated with known active myeloma only (2 NDMM, 2 RRMM; new fractures in 3/4 cases). Focal lesions were identified in 7 (19%) baseline scans (3 NDMM, 3 RRMM, 1 MGUS), mostly affecting spine and pelvis. Other findings included extraskeletal involvement (2/36), cord compression (1/36) and previous vertebral interventions (3/36 vertebroplasty, 1/36 stabilisation, 1/36 radiotherapy). Bone marrow appearance was normal in all HV scans, focal in 1/12 MGUS scans and otherwise normal, whereas a focal infiltrative pattern and an indeterminate pattern were demonstrated in 2/9 SMM cases. 4/9 of active myeloma cases showed a focal infiltrative pattern. For response assessment, no change was noticed in the patients with normal bone marrow pattern at baseline. No change was noticed in a patient with focal infiltrative pattern who received anti-myeloma treatment with lack of serological response, whereas two patients achieving a complete serological response were in the “highly likely to respond” category based on the change in bone marrow pattern and ADC measurement.
Conclusion
Using MYRADS recommendations, WB DW MRI serves as a good qualitative discriminator between HV/MGUS and myeloma patient cohorts. In the myeloma cohort, we validated MYRADS recommendations to demonstrate patterns of disease infiltration and disease response categorisation. We aim to report results at the meeting from a larger cohort in the ongoing study.
Keyword(s): Bone disease, MRI, Myeloma
Abstract: PB1671
Type: Publication Only
Session title: Myeloma and other monoclonal gammopathies - Clinical
Background
Cross-sectional MRI imaging has a growing importance in the classification of plasma cell dyscrasias, and in the definition of multiple myeloma (MM) response or progression (Dimopoulos 2015, Chantry 2017). High sensitivity of a diffusion-weighted whole body MRI (DW-WBMRI) in the early detection of bone marrow changes has been acknowledged in the revised IMWG diagnostic criteria (Rajkumar et al, 2014). A multidisciplinary imaging and haematologist expert panel has supported the measurement of cell density using an apparent diffusion coefficient (ADC) for the early diagnosis of changes in bone marrow infiltration and myeloma focal lesions (Messiou 2019). Recommendations for myeloma diagnosis and response assessment has been published (MYRADS) recently. We used data from a prospective plasma cell dyscrasias imaging study (NCT03951220) to validate these recommendations.
Aims
This prospective imaging study used a DW-MRI protocol to quantify longitudinal changes in tumour burden and bone disease. To improve sensitivity of bone marrow lesion identification healthy volunteers (HV) were also recruited. One of the study aims is to validate MYRADS protocol recommendations.
Methods
To validate the recommendations in the MYRADS protocol we took an unselected population of 18 MM pts, 12 MGUS pts and 6 HVs recruited between April 2018 and January 2019. See Table 1 for participants’ characteristics. After enrolment patients had a DW-WBMRI abbreviated protocol on the 3T Avanto MRI scanner (Siemens, Germany). In 18 participants with MM and MGUS the scan was repeated after 6 months using the same protocol. Qualitative assessment of bone marrow changes were made using the MYRADS recommendations. In each positive scan (Myeloma patients) we used the changes in ADC value (quantitative) of a single lytic lesion (MYRADS response assessment categories) and matched them with the serological parameters of disease.
Results
All 36 participants safely completed the protocol at baseline. Ten scans (28%) were positive for vertebral fractures (1 to 8 vertebral bodies involved); pathological fractures were associated with known active myeloma only (2 NDMM, 2 RRMM; new fractures in 3/4 cases). Focal lesions were identified in 7 (19%) baseline scans (3 NDMM, 3 RRMM, 1 MGUS), mostly affecting spine and pelvis. Other findings included extraskeletal involvement (2/36), cord compression (1/36) and previous vertebral interventions (3/36 vertebroplasty, 1/36 stabilisation, 1/36 radiotherapy). Bone marrow appearance was normal in all HV scans, focal in 1/12 MGUS scans and otherwise normal, whereas a focal infiltrative pattern and an indeterminate pattern were demonstrated in 2/9 SMM cases. 4/9 of active myeloma cases showed a focal infiltrative pattern. For response assessment, no change was noticed in the patients with normal bone marrow pattern at baseline. No change was noticed in a patient with focal infiltrative pattern who received anti-myeloma treatment with lack of serological response, whereas two patients achieving a complete serological response were in the “highly likely to respond” category based on the change in bone marrow pattern and ADC measurement.
Conclusion
Using MYRADS recommendations, WB DW MRI serves as a good qualitative discriminator between HV/MGUS and myeloma patient cohorts. In the myeloma cohort, we validated MYRADS recommendations to demonstrate patterns of disease infiltration and disease response categorisation. We aim to report results at the meeting from a larger cohort in the ongoing study.
Keyword(s): Bone disease, MRI, Myeloma


