
Contributions
Abstract: PB1656
Type: Publication Only
Session title: Myeloma and other monoclonal gammopathies - Clinical
Background
The detection of bone disease has important prognostic implications in multiple myeloma and can influence the diagnostic classification and the urgency of instituting treatment. Whole body magnetic resonance imaging (WB-MRI) is the most sensitive imaging technique and there are a number of advantages over other modalities. WB-MRI is able to detect axial and extra-axial disease, other solid organ malignancies, and has superior resolution and sensitivity for focal bone lesions. However, its use is restrained by a lack of local availability, paucity of radiological expertise in reporting, long acquisition time, and other factors. In this study, we hypothesised that more widespread use of WB-MRI would decrease the total number of scans, improve the patient journey and be cost effective.
Aims
The primary aim was to ascertain the feasibility, service impact and potential for cost-saving of instituting WB-MRI as the first-line skeletal imaging technique for patients with suspected or proven multiple myeloma in a large teaching hospital.
Methods
Electronic records of 88 consecutive patients with newly diagnosed multiple myeloma in the University Hospitals North Midlands NHS trust between 1st November 2018 and 31st October 2020 were studied. For the purposes of our analyses, a label of suspected myeloma was assigned when an abnormal protein electrophoresis or serum free light chain result was available. Confirmed myeloma was assigned when results of bone marrow showing >10% plasma cells was available. Data were anonymised and stored using Microsoft Excel on password-protected trust computers.
Results
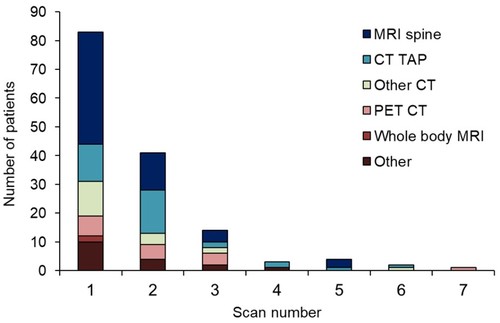
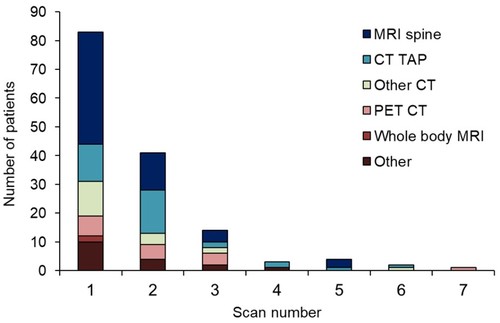
83 (94%) patients had imaging performed, with a total of 213 imaging procedures during the time period. Diagnostic imaging is summarised in figure 1 which includes all imaging performed prior, and up to, the achievement of a formal diagnosis of multiple myeloma (not follow-up scans). 43/83 (52%) had focal skeletal disease. Imaging triggered upstaging from smouldering myeloma to multiple myeloma in 7 (8%) patients. Where scans were performed for suspected or confirmed myeloma, 18 patients had in total 28 scans that could have been avoided if we had performed at the earliest realistic opportunity, 70 WB-MRI instead of 43 MRI whole spine, 12 computed tomography (CT) thorax, abdomen, and pelvis, 4 other CT scans, 8 positron emission tomography (PET) CT scans, and 3 other MRI scans. This equates to a direct cost saving of £11,428 (€13,177) over two-year period - a cost saving of £130 (€149) per patient – and the opportunity to redirect valuable scanner time for other cases.
Conclusion
As myeloma is a rare disease, patients arrive at the diagnosis through a variety of circuitous routes. It is therefore not feasible to perform WB-MRI in all patients as firstline imaging. However, it is reasonable to perform WB-MRI where myeloma is suspected or confirmed in place of other imaging. We have calculated direct cost savings but there are likely to be myriad benefits for the patient journey relating to improved diagnostic sensitivity and speed, fewer hospital visits, decreased exposure to radiation, and timely access to treatment where appropriate. Our findings support UK recommendations for WB-MRI as the first-line imaging modality. Radiology services should focus on expanding expertise in the delivery of this service and identifying patients who can benefit. Clinicians should be encouraged to utilise WB-MRI wherever possible.
Keyword(s): Cost effectiveness, MRI, Multiple myeloma
Abstract: PB1656
Type: Publication Only
Session title: Myeloma and other monoclonal gammopathies - Clinical
Background
The detection of bone disease has important prognostic implications in multiple myeloma and can influence the diagnostic classification and the urgency of instituting treatment. Whole body magnetic resonance imaging (WB-MRI) is the most sensitive imaging technique and there are a number of advantages over other modalities. WB-MRI is able to detect axial and extra-axial disease, other solid organ malignancies, and has superior resolution and sensitivity for focal bone lesions. However, its use is restrained by a lack of local availability, paucity of radiological expertise in reporting, long acquisition time, and other factors. In this study, we hypothesised that more widespread use of WB-MRI would decrease the total number of scans, improve the patient journey and be cost effective.
Aims
The primary aim was to ascertain the feasibility, service impact and potential for cost-saving of instituting WB-MRI as the first-line skeletal imaging technique for patients with suspected or proven multiple myeloma in a large teaching hospital.
Methods
Electronic records of 88 consecutive patients with newly diagnosed multiple myeloma in the University Hospitals North Midlands NHS trust between 1st November 2018 and 31st October 2020 were studied. For the purposes of our analyses, a label of suspected myeloma was assigned when an abnormal protein electrophoresis or serum free light chain result was available. Confirmed myeloma was assigned when results of bone marrow showing >10% plasma cells was available. Data were anonymised and stored using Microsoft Excel on password-protected trust computers.
Results
83 (94%) patients had imaging performed, with a total of 213 imaging procedures during the time period. Diagnostic imaging is summarised in figure 1 which includes all imaging performed prior, and up to, the achievement of a formal diagnosis of multiple myeloma (not follow-up scans). 43/83 (52%) had focal skeletal disease. Imaging triggered upstaging from smouldering myeloma to multiple myeloma in 7 (8%) patients. Where scans were performed for suspected or confirmed myeloma, 18 patients had in total 28 scans that could have been avoided if we had performed at the earliest realistic opportunity, 70 WB-MRI instead of 43 MRI whole spine, 12 computed tomography (CT) thorax, abdomen, and pelvis, 4 other CT scans, 8 positron emission tomography (PET) CT scans, and 3 other MRI scans. This equates to a direct cost saving of £11,428 (€13,177) over two-year period - a cost saving of £130 (€149) per patient – and the opportunity to redirect valuable scanner time for other cases.
Conclusion
As myeloma is a rare disease, patients arrive at the diagnosis through a variety of circuitous routes. It is therefore not feasible to perform WB-MRI in all patients as firstline imaging. However, it is reasonable to perform WB-MRI where myeloma is suspected or confirmed in place of other imaging. We have calculated direct cost savings but there are likely to be myriad benefits for the patient journey relating to improved diagnostic sensitivity and speed, fewer hospital visits, decreased exposure to radiation, and timely access to treatment where appropriate. Our findings support UK recommendations for WB-MRI as the first-line imaging modality. Radiology services should focus on expanding expertise in the delivery of this service and identifying patients who can benefit. Clinicians should be encouraged to utilise WB-MRI wherever possible.
Keyword(s): Cost effectiveness, MRI, Multiple myeloma


