
Contributions
Abstract: PB1639
Type: Publication Only
Session title: Myeloma and other monoclonal gammopathies - Biology & Translational Research
Background
Treatment for multiple myeloma (MM) is complex, involving several agents that may be used to induce and/or maintain response. While large electronic health databases (claims or electronic medical records [EMR]) represent sources of rich information on real-world use of these therapies and associated outcomes, they lack sufficient clinical detail needed to determine lines of therapy (LOTs) or treatment intent. Clinically robust and validated algorithms are required in order to use these data to identify LOTs—including when maintenance therapy (MT) is used and its constituent medication(s)—in MM.
Aims
To develop and assess performance of algorithms to identify LOTs among MM patients.
Methods
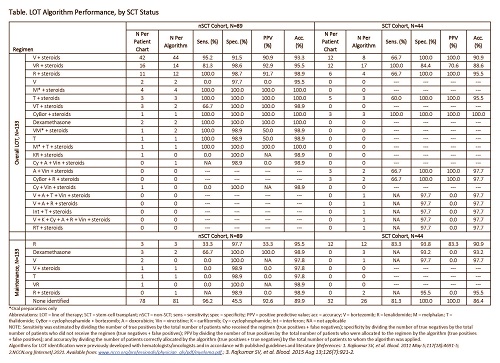
Algorithms for LOT identification were previously developed with hematologists/oncologists and in accordance with guidelines (Table). Validation of the algorithms was conducted using data from the Henry Ford Health System (HFHS). We identified adults with MM enrolled in the HFHS Health Alliance Plan (HAP) between January 1, 2006 and December 31, 2017. Patients whose HAP enrollment coincided with available medical chart data, and who had evidence of ≥1 “CRAB” (i.e., hypercalcemia, renal insufficiency, anemia, bone lesions) symptoms, were included. Starting from the date of the initial MM diagnosis, agents used to treat MM were identified in claims and EMR data. LOTs were then constituted based on the algorithms. First, individual agents were combined into small “mini-LOTs” using a series of defined rules (e.g., concomitant drugs) dependent on medications received. Next, mini-LOTs were combined into final LOTs based on additional rules that included: (1) receipt of ≥1 “new” agents of interest (not received in prior mini-LOT), including switches/augmentation; (2) days between mini-LOTs; (3) duration of prior mini-LOTs; and (4) whether the patient had undergone frontline stem-cell transplant (SCT). Attention was focused on the first LOT following diagnosis (LOT1). Use of MT within LOT1 was determined based on specific criteria, including duration and composition of mini-LOTs and SCT status. LOTs derived by these algorithms were then validated via review of all relevant clinical data in patients’ medical records by two independent hematologists/oncologists, with discordant cases adjudicated by a third arbitrator. Sensitivity, specificity, positive predictive value (PPV), and accuracy were estimated.
Results
A total of 133 patients (89 non-SCT [nSCT]; 44 SCT) were identified. Mean (standard deviation) age was 67.5 (11.6) years, 53.4% were male, and 60.9% were African American; 24.8%, 57.1%, 84.2%, and 39.1% had hypercalcemia, renal insufficiency, anemia, and bone lesions, respectively. The 3 most commonly used LOT1 regimens (Table) collectively represented 74.4% of patients. Overall accuracy of algorithms to identify LOT1 was 85.0% (88.8% nSCT; 77.3% SCT). For MT, it was 85.7% (87.6% nSCT; 81.8% SCT). PPVs for the most commonly used regimens ranged between 90.9%>92.9% for nSCT patients and 70.6%>100.0% for SCT patients. See the Table for validation statistics by regimens.
Conclusion
Algorithms to identify LOT1 and use of MT therein performed well, with an overall accuracy of 85.0% among patients with newly diagnosed MM. The algorithms performed numerically better in nSCT patients than SCT patients, although the latter had relatively smaller sample size. Further study in other large electronic healthcare databases is warranted to determine the consistency with which these algorithms can accurately constitute LOTs for the treatment of MM.
Keyword(s): Maintenance, Multiple myeloma, Therapy
Abstract: PB1639
Type: Publication Only
Session title: Myeloma and other monoclonal gammopathies - Biology & Translational Research
Background
Treatment for multiple myeloma (MM) is complex, involving several agents that may be used to induce and/or maintain response. While large electronic health databases (claims or electronic medical records [EMR]) represent sources of rich information on real-world use of these therapies and associated outcomes, they lack sufficient clinical detail needed to determine lines of therapy (LOTs) or treatment intent. Clinically robust and validated algorithms are required in order to use these data to identify LOTs—including when maintenance therapy (MT) is used and its constituent medication(s)—in MM.
Aims
To develop and assess performance of algorithms to identify LOTs among MM patients.
Methods
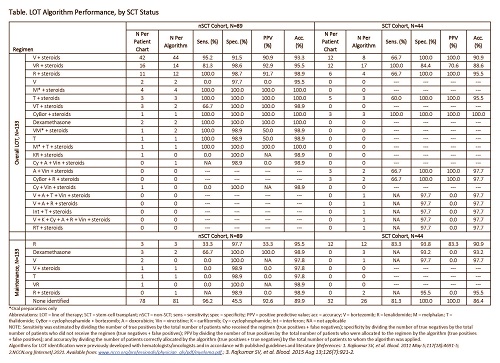
Algorithms for LOT identification were previously developed with hematologists/oncologists and in accordance with guidelines (Table). Validation of the algorithms was conducted using data from the Henry Ford Health System (HFHS). We identified adults with MM enrolled in the HFHS Health Alliance Plan (HAP) between January 1, 2006 and December 31, 2017. Patients whose HAP enrollment coincided with available medical chart data, and who had evidence of ≥1 “CRAB” (i.e., hypercalcemia, renal insufficiency, anemia, bone lesions) symptoms, were included. Starting from the date of the initial MM diagnosis, agents used to treat MM were identified in claims and EMR data. LOTs were then constituted based on the algorithms. First, individual agents were combined into small “mini-LOTs” using a series of defined rules (e.g., concomitant drugs) dependent on medications received. Next, mini-LOTs were combined into final LOTs based on additional rules that included: (1) receipt of ≥1 “new” agents of interest (not received in prior mini-LOT), including switches/augmentation; (2) days between mini-LOTs; (3) duration of prior mini-LOTs; and (4) whether the patient had undergone frontline stem-cell transplant (SCT). Attention was focused on the first LOT following diagnosis (LOT1). Use of MT within LOT1 was determined based on specific criteria, including duration and composition of mini-LOTs and SCT status. LOTs derived by these algorithms were then validated via review of all relevant clinical data in patients’ medical records by two independent hematologists/oncologists, with discordant cases adjudicated by a third arbitrator. Sensitivity, specificity, positive predictive value (PPV), and accuracy were estimated.
Results
A total of 133 patients (89 non-SCT [nSCT]; 44 SCT) were identified. Mean (standard deviation) age was 67.5 (11.6) years, 53.4% were male, and 60.9% were African American; 24.8%, 57.1%, 84.2%, and 39.1% had hypercalcemia, renal insufficiency, anemia, and bone lesions, respectively. The 3 most commonly used LOT1 regimens (Table) collectively represented 74.4% of patients. Overall accuracy of algorithms to identify LOT1 was 85.0% (88.8% nSCT; 77.3% SCT). For MT, it was 85.7% (87.6% nSCT; 81.8% SCT). PPVs for the most commonly used regimens ranged between 90.9%>92.9% for nSCT patients and 70.6%>100.0% for SCT patients. See the Table for validation statistics by regimens.
Conclusion
Algorithms to identify LOT1 and use of MT therein performed well, with an overall accuracy of 85.0% among patients with newly diagnosed MM. The algorithms performed numerically better in nSCT patients than SCT patients, although the latter had relatively smaller sample size. Further study in other large electronic healthcare databases is warranted to determine the consistency with which these algorithms can accurately constitute LOTs for the treatment of MM.
Keyword(s): Maintenance, Multiple myeloma, Therapy


