
Contributions
Abstract: PB1594
Type: Publication Only
Session title: Infections in hematology (incl. supportive care/therapy)
Background
Pulmonary infections occur frequently during the management of patients with hematologic malignancies, and usually managed with empirical strategy before the responsible pathogen could be identified. However, conventional techniques such as culture are not sensitive enough and have a long turnaround time. If a patient failed multiple lines of anti-microbial treatment or had an exacerbation of infection, then a rapid and effective way to identify responsible pathogen is critical. Next-generation sequencing (NGS) has the potential to detect pathogenic microbe in a high throughout and rapid way, which is different from the conventional techniques in this respect. However, when and who to integrate NGS into management of pulmonary infection is currently unclear.
Aims
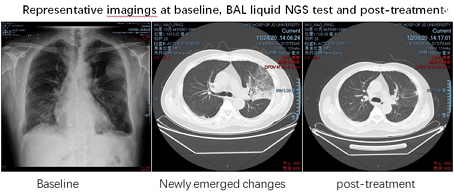
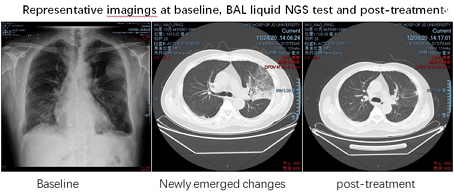
To explore the feasibility and effectiveness of next-generation sequencing (NGS) test to identify responsible microbial pathogens in bronchoscopic bronchoalveolar lavage (BAL) liquid, which was obtained from febrile patients who both failed multiple lines of antimicrobial therapy and had newly emerged pulmonary changes on X-rays or CT scan.
Methods
All the patients had received anti-cancer therapy of underlying hematologic malignancies before infections developed. If a patient developed febrile episodes and still had persistent or recurrent fever even with multiple lines of empirical anti-microbial treatment, once newly emerged pulmonary changes on X-rays or CT scan were documented, bronchoscopic bronchoalveolar lavage (BAL) liquid was then obtained for NGS test. When the definitive microbial pathogen is identified, specific antimicrobial strategy was employed accordingly.
Results
All four cases had been treated for underlying hematologic malignancies in our hospital, two of them for acute lymphoblastic leukemia and the other two cases for multiple myeloma. During the anti-malignancy treatment, all had febrile neutropenia (FN) and received multiple lines of antimicrobial treatment. Even with rigorous combined and multiple lines of antimicrobial agent treatment, three of them had persistent fever and the fourth had recurrent fever. All cases had baseline pulmonary imaging scan and a routine imaging follow-up was employed during anti-microbial treatment. As soon as a newly emerged change was confirmed by either X-rays or CT scan, bronchoscopic BAL liquid was obtained for NGS test in an attempt to identify responsible pathogen. All cases had negative blood and sputum culture, negative galactomannan (GM) and β-D-Glucan assay (G) test before bronchoscope. NGS test had positive findings in all four cases, the pathogens are Lautropia mirabilis, Aspergillus fumigates, Pneumocystis jirovecii and Aspergillus fumigates, respectively. Only one case had subsequent positive serum GM assay and sputum Aspergillus fumigates detection after NGS test. Every case had the antimicrobial agents adjusted according to NGS results, and fever resolved in all cases. Subsequent imaging showed significantly improved or resolved in all four cases.
Conclusion
In the management of refractory/recurrent pulmonary infection patients with hematological malignancies, NGS test of bronchoscopic BAL liquid should be considered if previous conventional test cannot identify pathogen, especially when there are newly emerged changes on X-rays or CT scan.
Keyword(s): Infection, Pulmonary
Abstract: PB1594
Type: Publication Only
Session title: Infections in hematology (incl. supportive care/therapy)
Background
Pulmonary infections occur frequently during the management of patients with hematologic malignancies, and usually managed with empirical strategy before the responsible pathogen could be identified. However, conventional techniques such as culture are not sensitive enough and have a long turnaround time. If a patient failed multiple lines of anti-microbial treatment or had an exacerbation of infection, then a rapid and effective way to identify responsible pathogen is critical. Next-generation sequencing (NGS) has the potential to detect pathogenic microbe in a high throughout and rapid way, which is different from the conventional techniques in this respect. However, when and who to integrate NGS into management of pulmonary infection is currently unclear.
Aims
To explore the feasibility and effectiveness of next-generation sequencing (NGS) test to identify responsible microbial pathogens in bronchoscopic bronchoalveolar lavage (BAL) liquid, which was obtained from febrile patients who both failed multiple lines of antimicrobial therapy and had newly emerged pulmonary changes on X-rays or CT scan.
Methods
All the patients had received anti-cancer therapy of underlying hematologic malignancies before infections developed. If a patient developed febrile episodes and still had persistent or recurrent fever even with multiple lines of empirical anti-microbial treatment, once newly emerged pulmonary changes on X-rays or CT scan were documented, bronchoscopic bronchoalveolar lavage (BAL) liquid was then obtained for NGS test. When the definitive microbial pathogen is identified, specific antimicrobial strategy was employed accordingly.
Results
All four cases had been treated for underlying hematologic malignancies in our hospital, two of them for acute lymphoblastic leukemia and the other two cases for multiple myeloma. During the anti-malignancy treatment, all had febrile neutropenia (FN) and received multiple lines of antimicrobial treatment. Even with rigorous combined and multiple lines of antimicrobial agent treatment, three of them had persistent fever and the fourth had recurrent fever. All cases had baseline pulmonary imaging scan and a routine imaging follow-up was employed during anti-microbial treatment. As soon as a newly emerged change was confirmed by either X-rays or CT scan, bronchoscopic BAL liquid was obtained for NGS test in an attempt to identify responsible pathogen. All cases had negative blood and sputum culture, negative galactomannan (GM) and β-D-Glucan assay (G) test before bronchoscope. NGS test had positive findings in all four cases, the pathogens are Lautropia mirabilis, Aspergillus fumigates, Pneumocystis jirovecii and Aspergillus fumigates, respectively. Only one case had subsequent positive serum GM assay and sputum Aspergillus fumigates detection after NGS test. Every case had the antimicrobial agents adjusted according to NGS results, and fever resolved in all cases. Subsequent imaging showed significantly improved or resolved in all four cases.
Conclusion
In the management of refractory/recurrent pulmonary infection patients with hematological malignancies, NGS test of bronchoscopic BAL liquid should be considered if previous conventional test cannot identify pathogen, especially when there are newly emerged changes on X-rays or CT scan.
Keyword(s): Infection, Pulmonary


