
Contributions
Abstract: PB1590
Type: Publication Only
Session title: Infections in hematology (incl. supportive care/therapy)
Background
Bacterial bloodstream infections (BSI) have a significant impact on treatment outcomes in patients with acute myeloid leukemia (AML). According to P. Kalaskar et al. the incidence of BSI during the induction phase is 27.8%, and during consolidation phase is about 25%.
Aims
To explore the epidemiological characteristics and risk factors of BSI in patients with AML, who develop agranulocytosis fever after chemotherapy.
Methods
A retrospective analysis of 221 patients with AML, 26 of which were diagnosed with AML for the first time in 2020, treated in the Department of Hematology of our hospital, was conducted from January 2020 to August 2020 to analyze the incidence of BSI, the distribution and types of pathogenic bacteria. We also determined whether various parameters are risk factors to BSI, including the patient age, gender, agranulocytosis time, the absolute value of neutrophils on the day of agranular fever.
Results
Among the 221 patients, 37 (16.7%) had agranulocytosis fever and were microbiologically confirmed as BSIs, including 17 (65.3%) who were diagnosed for the first time. The patients included 16 (43.3%) males and 21 (56.7%) females, with median age of 44 years (21-71).
Nine pathogens were detected in 37 patients, including 4 G-strains (86.4%) and 5 G+ bacteria (13.6%). Following pathogens were noted: K. pneumoniae - in 18 (48.6%), E. coli - in 12 (32.4%), A. baumannii - in 1 (2.7%), E. cloacae - in 1 (2.7%), S. Haemolyticus - in 1 (2.7%), S. hominis - in 1 (2.7%), S. epidermidis - in 2 (5.4%), S. aureus - in 1 (2.7 %), E. faecalis - in 1 (2.7%).
Also, in several patients, different pathogens of BSI were isolated during one hospitalization. Agranulocytosis was registered in all patients on the day of BSI, of which 34 (91.8%) had absolute value of neutrophils less than 0.2 * 109 / L.
As an empiric antibiotic therapy, in 29.7% of cases, a combination of a 4th generation cephalosporin (cefepime) with a 3rd generation aminoglycoside (amikacin) was used, and in 70.3% of cases, a combination of carbapenem (meropenem) with a 3rd generation aminoglycoside (amikacin), while empirical antibiotic therapy was rational in 35.1% of cases, escalation was required in 64.8% of cases.In 86.4% of cases, the outcome of therapy showed stabilization of the patient's condition and in 13.6% of cases, a lethal outcome was registered.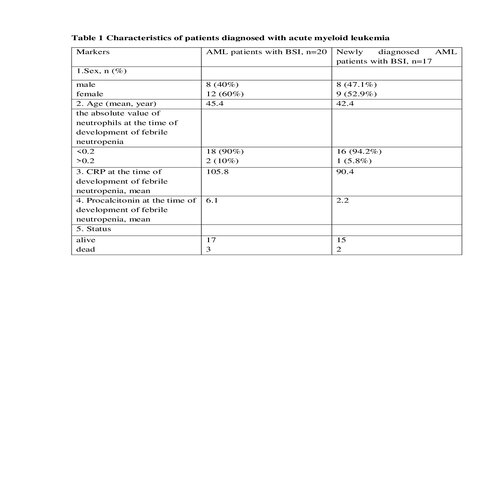
Conclusion
1. In the etiological spectrum of pathogens of bloodstream infections in patients with AML, gram-negative pathogens (86.4%) predominate, mainly of endogenous, most likely intestinal origin.2. Repetitive cases of bloodstream infections caused by different pathogens during the same hospitalization were noted.3. In more than 90% of patients with AML and bloodstream infection, this infectious complication was observed with absolute value of neutrophils below 0.2 * 109/ L.
95% CI was 91.9% (78.7% -97.2%)4. All deceased patients had absolute value of neutrophils below 0.2 * 109/ L.
Keyword(s): Acute myeloid leukemia, Infection, Pathogen reduction
Abstract: PB1590
Type: Publication Only
Session title: Infections in hematology (incl. supportive care/therapy)
Background
Bacterial bloodstream infections (BSI) have a significant impact on treatment outcomes in patients with acute myeloid leukemia (AML). According to P. Kalaskar et al. the incidence of BSI during the induction phase is 27.8%, and during consolidation phase is about 25%.
Aims
To explore the epidemiological characteristics and risk factors of BSI in patients with AML, who develop agranulocytosis fever after chemotherapy.
Methods
A retrospective analysis of 221 patients with AML, 26 of which were diagnosed with AML for the first time in 2020, treated in the Department of Hematology of our hospital, was conducted from January 2020 to August 2020 to analyze the incidence of BSI, the distribution and types of pathogenic bacteria. We also determined whether various parameters are risk factors to BSI, including the patient age, gender, agranulocytosis time, the absolute value of neutrophils on the day of agranular fever.
Results
Among the 221 patients, 37 (16.7%) had agranulocytosis fever and were microbiologically confirmed as BSIs, including 17 (65.3%) who were diagnosed for the first time. The patients included 16 (43.3%) males and 21 (56.7%) females, with median age of 44 years (21-71).
Nine pathogens were detected in 37 patients, including 4 G-strains (86.4%) and 5 G+ bacteria (13.6%). Following pathogens were noted: K. pneumoniae - in 18 (48.6%), E. coli - in 12 (32.4%), A. baumannii - in 1 (2.7%), E. cloacae - in 1 (2.7%), S. Haemolyticus - in 1 (2.7%), S. hominis - in 1 (2.7%), S. epidermidis - in 2 (5.4%), S. aureus - in 1 (2.7 %), E. faecalis - in 1 (2.7%).
Also, in several patients, different pathogens of BSI were isolated during one hospitalization. Agranulocytosis was registered in all patients on the day of BSI, of which 34 (91.8%) had absolute value of neutrophils less than 0.2 * 109 / L.
As an empiric antibiotic therapy, in 29.7% of cases, a combination of a 4th generation cephalosporin (cefepime) with a 3rd generation aminoglycoside (amikacin) was used, and in 70.3% of cases, a combination of carbapenem (meropenem) with a 3rd generation aminoglycoside (amikacin), while empirical antibiotic therapy was rational in 35.1% of cases, escalation was required in 64.8% of cases.In 86.4% of cases, the outcome of therapy showed stabilization of the patient's condition and in 13.6% of cases, a lethal outcome was registered.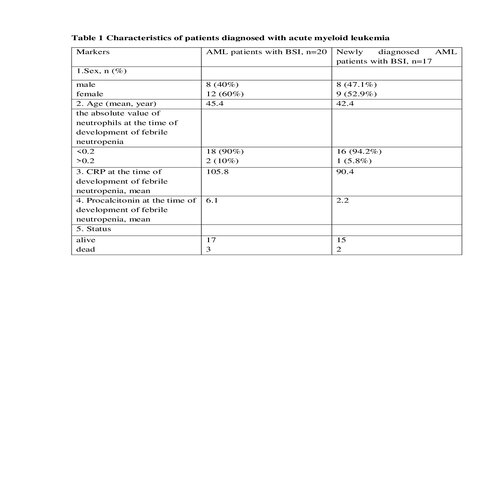
Conclusion
1. In the etiological spectrum of pathogens of bloodstream infections in patients with AML, gram-negative pathogens (86.4%) predominate, mainly of endogenous, most likely intestinal origin.2. Repetitive cases of bloodstream infections caused by different pathogens during the same hospitalization were noted.3. In more than 90% of patients with AML and bloodstream infection, this infectious complication was observed with absolute value of neutrophils below 0.2 * 109/ L.
95% CI was 91.9% (78.7% -97.2%)4. All deceased patients had absolute value of neutrophils below 0.2 * 109/ L.
Keyword(s): Acute myeloid leukemia, Infection, Pathogen reduction


