
Contributions
Abstract: PB1584
Type: Publication Only
Session title: Infections in hematology (incl. supportive care/therapy)
Background
The novel coronavirus SARS-CoV-2 was officially detected in Spain on January 31, 2020. Since then, the health system has suffered 3 waves of healthcare pressure due to this pandemic infection. There was concern about the impact of Coronavirus 2019 disease (COVID-19) being significant in haematological patients.
Aims
Find out the mortality rate by COVID-19 in a cohort of hematological patients.
Identify potential predictive parameters associated with poor outcome in patients with a diagnosis of haematological malignancy and COVID-19.
Methods
Retrospective and descriptive study of hospitalized patients in the Hematology Clinical Management Unit at our center, between February 12, 2020 and February 12, 2021. The patients had a diagnosis of a haematological malignancy and laboratory-confirmed COVID-19. We performed a Pearson correlation test on Phyton between variables of interest.
Results
356 patients were admitted in the Hematology Unit in the referred period.
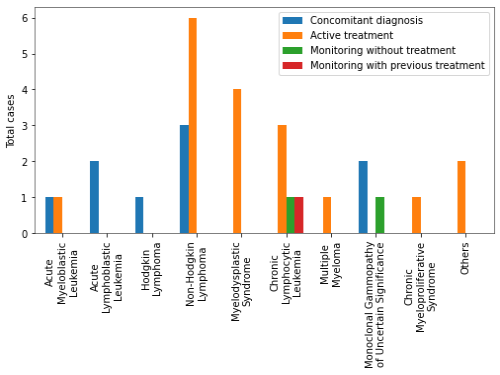
Of these, 30 had SARS-CoV-2 infection on arrival or during their hospital stay (10% nosocomial infection rate). We summarize in Table 1 total cases reported by diagnostic and state.
There was a male predominance (69%), with a median age of 67 years old [14-90]. Average days of symptom onset until admission: 7.81 days. Chest X-ray images at the diagnosis: bilateral pneumonia (37.9%), peripheral infiltrates (13.8%), unilateral infiltrates (17.2%).
Patients were treated according to local guidelines with high-dose corticosteroid pulses, remdesivir and interleukin inhibitors. Only 13,3% of them needed additional support in the Intensive Care Unit.
Mortality rate in our cohort was 30%. The mortality rate at our hospital for patients with COVID-19 and no haematological malignancy within the same period of time was 10%. By subgroups, non-Hodgkin's lymphoma (NHL) group was the neoplasm with largest number of deaths. 62.5% of these patients had a 4C Mortality Score between 1 and 8 points, ranking in the intermediate risk group. 55.56% (5/9) of them expired. Myelodysplastic syndrome (MDS) group had the highest 4C Mortality Score, with more than 10 points, placing itself in the high or very high-risk group. 50% (2/4) of them died.
We have found no correlation between the level of ferritin, Interleukin 6 (IL6), neutrophils, monocytes, platelets, D-dimer and successive clinical and radiological evolution in these patients, in contrast with other studies in the general population. We found a weakly positive relationship between the IL6 level at admission and the subsequent need to enter in the Intensive Care Unit (r= 0.44, p<0.05). We noticed a negative correlation between the IL6 level at admission and clinical improvement after treatment by protocol (r =-0.21 p<0.05), the day of symptom evolution at admission and age (r= -0.58 p< 0.05).
Conclusion
- SARS-CoV2 infection incidence in our cohort was lower than expected, but the mortality rate was superior compared to hospitalized patients with no haematological malignancy.
- MDS group had the highest risk according to the 4C Mortality Score, with 50% of the patients dying due to the infection in our study. We think it may be related to older patients with more comorbidities. Mortality rate was also high in patients with NHL in spite of lower potential risk. Further prognostic scores should be developed in order to properly predict the risk of poor outcome in hematological patients.
- IL-6 seems to be a key component of the immune response to SARS-CoV-2 as well as clinical evolution, even in immunocompromised patients.
Keyword(s): COVID-19, Hematological malignancy, Mortality
Abstract: PB1584
Type: Publication Only
Session title: Infections in hematology (incl. supportive care/therapy)
Background
The novel coronavirus SARS-CoV-2 was officially detected in Spain on January 31, 2020. Since then, the health system has suffered 3 waves of healthcare pressure due to this pandemic infection. There was concern about the impact of Coronavirus 2019 disease (COVID-19) being significant in haematological patients.
Aims
Find out the mortality rate by COVID-19 in a cohort of hematological patients.
Identify potential predictive parameters associated with poor outcome in patients with a diagnosis of haematological malignancy and COVID-19.
Methods
Retrospective and descriptive study of hospitalized patients in the Hematology Clinical Management Unit at our center, between February 12, 2020 and February 12, 2021. The patients had a diagnosis of a haematological malignancy and laboratory-confirmed COVID-19. We performed a Pearson correlation test on Phyton between variables of interest.
Results
356 patients were admitted in the Hematology Unit in the referred period.
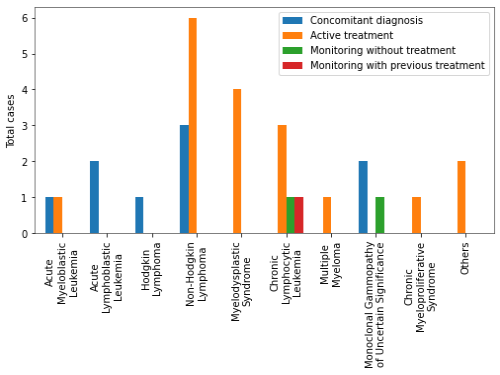
Of these, 30 had SARS-CoV-2 infection on arrival or during their hospital stay (10% nosocomial infection rate). We summarize in Table 1 total cases reported by diagnostic and state.
There was a male predominance (69%), with a median age of 67 years old [14-90]. Average days of symptom onset until admission: 7.81 days. Chest X-ray images at the diagnosis: bilateral pneumonia (37.9%), peripheral infiltrates (13.8%), unilateral infiltrates (17.2%).
Patients were treated according to local guidelines with high-dose corticosteroid pulses, remdesivir and interleukin inhibitors. Only 13,3% of them needed additional support in the Intensive Care Unit.
Mortality rate in our cohort was 30%. The mortality rate at our hospital for patients with COVID-19 and no haematological malignancy within the same period of time was 10%. By subgroups, non-Hodgkin's lymphoma (NHL) group was the neoplasm with largest number of deaths. 62.5% of these patients had a 4C Mortality Score between 1 and 8 points, ranking in the intermediate risk group. 55.56% (5/9) of them expired. Myelodysplastic syndrome (MDS) group had the highest 4C Mortality Score, with more than 10 points, placing itself in the high or very high-risk group. 50% (2/4) of them died.
We have found no correlation between the level of ferritin, Interleukin 6 (IL6), neutrophils, monocytes, platelets, D-dimer and successive clinical and radiological evolution in these patients, in contrast with other studies in the general population. We found a weakly positive relationship between the IL6 level at admission and the subsequent need to enter in the Intensive Care Unit (r= 0.44, p<0.05). We noticed a negative correlation between the IL6 level at admission and clinical improvement after treatment by protocol (r =-0.21 p<0.05), the day of symptom evolution at admission and age (r= -0.58 p< 0.05).
Conclusion
- SARS-CoV2 infection incidence in our cohort was lower than expected, but the mortality rate was superior compared to hospitalized patients with no haematological malignancy.
- MDS group had the highest risk according to the 4C Mortality Score, with 50% of the patients dying due to the infection in our study. We think it may be related to older patients with more comorbidities. Mortality rate was also high in patients with NHL in spite of lower potential risk. Further prognostic scores should be developed in order to properly predict the risk of poor outcome in hematological patients.
- IL-6 seems to be a key component of the immune response to SARS-CoV-2 as well as clinical evolution, even in immunocompromised patients.
Keyword(s): COVID-19, Hematological malignancy, Mortality


