
Contributions
Abstract: PB1580
Type: Publication Only
Session title: Indolent and mantle-cell non-Hodgkin lymphoma - Clinical
Background
Mantle Cell Lymphoma (MCL) is a rare type of non-Hodgkin lymphoma (NHL), with an aggressive clinical course. MCL is associated with poor prognosis and incurable disease in the majority of the patients. However, a minority of patients will not require any treatment for many years. Although MCL is initially responsive to different conventional chemotherapies, such a response is short-lived. The median overall survival in modern trials incorporating intensive therapy has improved accounting of 8 to 10 years. However TP53 mutation continue to confers a dismal prognosis in MCL with a median survival of 1.3 years. Targeted therapy and recently more promising CAR-T therapy have revolutionized this disease out-come.
Aims
This is a single-centre, retrospective analysis of MCL patients treated over study period (2006-2020) to evaluate our MCL patients treatment out-come.
Methods
Using our MCL data-base, baseline patient’s demographic characteristics, clinical features, laboratory findings, MIPI score, initial/subsequent treatment responses and survival were analysed. Patient's informed consent was obtained. Sub-set of patients have completed p53 disruption screen using both p53 expression on immuno-histochemistry (IHC) and mutational status and this genetic defect impact was evaluated here.
Results
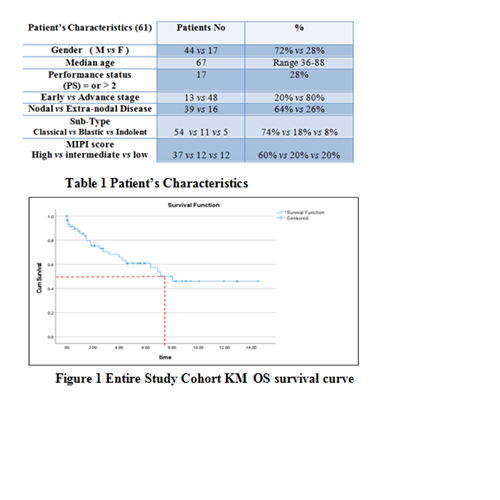
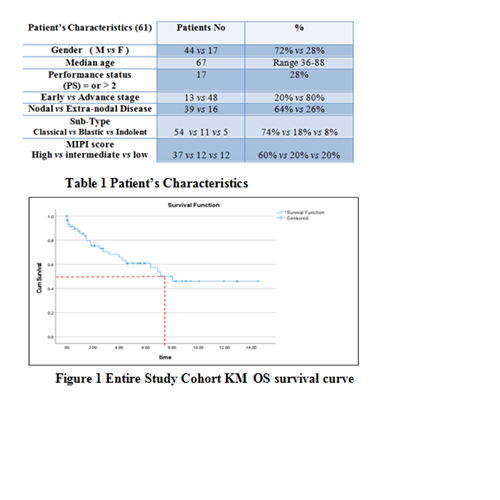
Sixty-one patients were included in this study, with male predominance, median age 67 yrers and the majority with advanced disease. 50% presented with B symptoms and BM involvement in 35 (57%) patients (Table 1). Chemo-immunotherapy (CIT) remains the main treatment modality in our cohort (54/88% patients), resulted in an ORR of 79%, CR 55% and PR 24%, which compares well with the reported literature. 5 (8%) patients were not eligible for any treatment, one patient received IFRT only for early-stage disease and one patient had splenectomy. Rituximab maintenance was used in 29 (48%) and 3 (5%) patient had ASCT. 21 (39%) patients had relapsed disease,11(52%) patients treated with Ibrutinib as a second line, 7 (33%) patients treated with CIT, with one (5%) patient with HL relapse treated with ABVD and 2 (10%) patients were not suitable for further treatment. Eight (38%) experienced further disease relapse, 3 (14%) patients received Ibrutinib and 5 (23%) patient received CIT and 1 (1.6%) patient had Allo-SCT. At time of the study analysis, 40 (67%) patients were still alive and 23 (38%) patients had died. The median survival for all the cohort was 3 years (range 0-14 years). To date, 29 (46%) patient’s samples screened for p53 disruptions, only 6 (10%) patient’s sample demonstrate a high p53 expression and harboured deleterious TP53 mutation by NGS sequencing. Most of MCL cases harbouring TP53 mutations have an aggressive disease course with multiple disease relapses and lymphoma related deaths (80%). In sub-set analyses, the OS was only 4 years in TP53 mutated disease and was not reached in wild-type TP53 cohort (P value = 0.007, log rank test) which is comparable to the reported data. The median overall survival (OS) for the entire cohort was 7 years (Fig 1), according to disease sub-type classic vs blastic , the median survival were 8 years vs 2 years respectively.
Conclusion
Mantle cell lymphoma (MCL) continue to be challenging disease to treat with a short lived treatment response and frequent relapses. Genetic risk stratification and clinical trials enrollement are of great importance. Our data showed comparable treatment outcome similar to the reported literatures.
Keyword(s): Chemotherapy, Mantle cell lymphoma, Outcome, P53
Abstract: PB1580
Type: Publication Only
Session title: Indolent and mantle-cell non-Hodgkin lymphoma - Clinical
Background
Mantle Cell Lymphoma (MCL) is a rare type of non-Hodgkin lymphoma (NHL), with an aggressive clinical course. MCL is associated with poor prognosis and incurable disease in the majority of the patients. However, a minority of patients will not require any treatment for many years. Although MCL is initially responsive to different conventional chemotherapies, such a response is short-lived. The median overall survival in modern trials incorporating intensive therapy has improved accounting of 8 to 10 years. However TP53 mutation continue to confers a dismal prognosis in MCL with a median survival of 1.3 years. Targeted therapy and recently more promising CAR-T therapy have revolutionized this disease out-come.
Aims
This is a single-centre, retrospective analysis of MCL patients treated over study period (2006-2020) to evaluate our MCL patients treatment out-come.
Methods
Using our MCL data-base, baseline patient’s demographic characteristics, clinical features, laboratory findings, MIPI score, initial/subsequent treatment responses and survival were analysed. Patient's informed consent was obtained. Sub-set of patients have completed p53 disruption screen using both p53 expression on immuno-histochemistry (IHC) and mutational status and this genetic defect impact was evaluated here.
Results
Sixty-one patients were included in this study, with male predominance, median age 67 yrers and the majority with advanced disease. 50% presented with B symptoms and BM involvement in 35 (57%) patients (Table 1). Chemo-immunotherapy (CIT) remains the main treatment modality in our cohort (54/88% patients), resulted in an ORR of 79%, CR 55% and PR 24%, which compares well with the reported literature. 5 (8%) patients were not eligible for any treatment, one patient received IFRT only for early-stage disease and one patient had splenectomy. Rituximab maintenance was used in 29 (48%) and 3 (5%) patient had ASCT. 21 (39%) patients had relapsed disease,11(52%) patients treated with Ibrutinib as a second line, 7 (33%) patients treated with CIT, with one (5%) patient with HL relapse treated with ABVD and 2 (10%) patients were not suitable for further treatment. Eight (38%) experienced further disease relapse, 3 (14%) patients received Ibrutinib and 5 (23%) patient received CIT and 1 (1.6%) patient had Allo-SCT. At time of the study analysis, 40 (67%) patients were still alive and 23 (38%) patients had died. The median survival for all the cohort was 3 years (range 0-14 years). To date, 29 (46%) patient’s samples screened for p53 disruptions, only 6 (10%) patient’s sample demonstrate a high p53 expression and harboured deleterious TP53 mutation by NGS sequencing. Most of MCL cases harbouring TP53 mutations have an aggressive disease course with multiple disease relapses and lymphoma related deaths (80%). In sub-set analyses, the OS was only 4 years in TP53 mutated disease and was not reached in wild-type TP53 cohort (P value = 0.007, log rank test) which is comparable to the reported data. The median overall survival (OS) for the entire cohort was 7 years (Fig 1), according to disease sub-type classic vs blastic , the median survival were 8 years vs 2 years respectively.
Conclusion
Mantle cell lymphoma (MCL) continue to be challenging disease to treat with a short lived treatment response and frequent relapses. Genetic risk stratification and clinical trials enrollement are of great importance. Our data showed comparable treatment outcome similar to the reported literatures.
Keyword(s): Chemotherapy, Mantle cell lymphoma, Outcome, P53


