
Contributions
Abstract: PB1568
Type: Publication Only
Session title: Indolent and mantle-cell non-Hodgkin lymphoma - Clinical
Background
Most follicular lymphoma (FL) patients have prolonged survival. However, early progression (POD24) and histological transformation (HT) compromise their life expectancy. With the intention of identifying such individuals, different risk scores (RS) have been developed. Although FLIPI has gained the widest acceptance, none of the previous (IPI, ILI) or more recent indexes (FLIPI2, PRIMA-PI) has been clearly shown to outperform the others.
Aims
To evaluate the utility of the IPI, ILI, FLIPI, FLIPI2, and PRIMA-PI in a single-center series of FL patients.
Methods
We studied 414 grade 1-3A FL patients [230 F/184 M; median age, 60 years (range, 26−91)] who had available information about at least one of the five clinical RS (IPI, ILI, FLIPI, FLIPI2, PRIMA-PI), diagnosed at our institution between 2002 and 2018. Three hundred and ten patients (75%) had advanced-stage disease, and 250 (69%) received frontline treatment with R-CHOP or R-CVP. With a median follow-up of 5.9 years, 10-year overall survival (OS) was 71%.
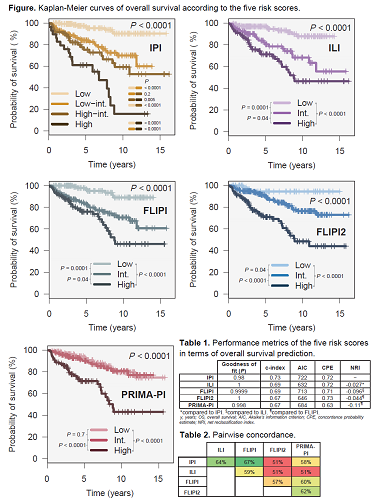
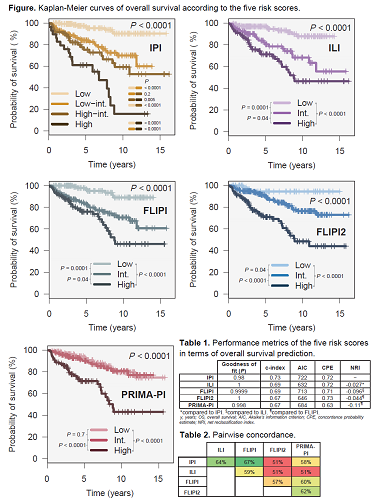
Prognostic performance of each RS was evaluated in terms of calibration (Hosmer-Lemeshow goodness of fit), discrimination [Harrell’s c-index, Akaike’s information criterion (AIC), and Gönen & Heller’s concordance probability estimate (CPE)], reclassification [net reclassification index (NRI)], and clinical utility [prediction of time to first treatment (TTFT), response, progression-free survival (PFS), OS, risk of lymphoma related death (LRD), and of HT].
Results
Performance metrics of the five RS are detailed in Table 1. Goodness of fit, Harrell’s c-index, AIC, and CPE were similar across indexes. NRI did not show improvement of any RS in comparison with the existing ones. The proportion of patients allocated to the high-risk category by each RS was as follows: 7% (IPI), 27% (ILI), 28% (FLIPI), 30% (FLIPI2), and 27% (PRIMA-PI). Pairwise concordance (patients allocated to the same risk category by two RS, Table 2) was lowest between IPI-FLIPI2, ILI-FLIPI2, and ILI-PRIMA-PI (51%), and highest between IPI-FLIPI (67%). All five RS predicted TTFT (P <0.01). Using logistic regression, all five RS predicted for the absence of complete response, as well as for POD24.
All five RS were predictive of PFS (P <0.0001), OS (P <0.0001, Figure), and LRD (P <0.001). Ten-year OS estimates for each high-risk group were as follows: 16% (IPI), 46% (ILI), 46% (FLIPI), 48% (FLIPI2), 43% (PRIMA-PI). Although PRIMA-PI identified a high-risk group (B2M >3 mg/L), no significant differences in OS were found according to bone marrow infiltration (pairwise P = 0.7). FLIPI was the only RS to predict HT, with 10-y cumulative incidences of 3%, 8% and 10% for low-, intermediate-, and high-risk patients, respectively (P = 0.04).
Conclusion
The five RS exhibit very subtle differences in their performance metrics. All of them predict TTFT, response, POD24, PFS, OS, and the risk of LRD. IPI identifies a small subset of patients with dismal outcomes. Bone marrow involvement did not impact OS, questioning the prognostic discrimination of the low- and intermediate-risk PRIMA-PI categories. In our series, FLIPI was the only RS to predict HT. In summary, all available RS are similarly valid for prognostication. Their potential to aid in the decision of initiating treatment should be explored.
Keyword(s): Follicular lymphoma, Prognostic groups, Survival prediction
Abstract: PB1568
Type: Publication Only
Session title: Indolent and mantle-cell non-Hodgkin lymphoma - Clinical
Background
Most follicular lymphoma (FL) patients have prolonged survival. However, early progression (POD24) and histological transformation (HT) compromise their life expectancy. With the intention of identifying such individuals, different risk scores (RS) have been developed. Although FLIPI has gained the widest acceptance, none of the previous (IPI, ILI) or more recent indexes (FLIPI2, PRIMA-PI) has been clearly shown to outperform the others.
Aims
To evaluate the utility of the IPI, ILI, FLIPI, FLIPI2, and PRIMA-PI in a single-center series of FL patients.
Methods
We studied 414 grade 1-3A FL patients [230 F/184 M; median age, 60 years (range, 26−91)] who had available information about at least one of the five clinical RS (IPI, ILI, FLIPI, FLIPI2, PRIMA-PI), diagnosed at our institution between 2002 and 2018. Three hundred and ten patients (75%) had advanced-stage disease, and 250 (69%) received frontline treatment with R-CHOP or R-CVP. With a median follow-up of 5.9 years, 10-year overall survival (OS) was 71%.
Prognostic performance of each RS was evaluated in terms of calibration (Hosmer-Lemeshow goodness of fit), discrimination [Harrell’s c-index, Akaike’s information criterion (AIC), and Gönen & Heller’s concordance probability estimate (CPE)], reclassification [net reclassification index (NRI)], and clinical utility [prediction of time to first treatment (TTFT), response, progression-free survival (PFS), OS, risk of lymphoma related death (LRD), and of HT].
Results
Performance metrics of the five RS are detailed in Table 1. Goodness of fit, Harrell’s c-index, AIC, and CPE were similar across indexes. NRI did not show improvement of any RS in comparison with the existing ones. The proportion of patients allocated to the high-risk category by each RS was as follows: 7% (IPI), 27% (ILI), 28% (FLIPI), 30% (FLIPI2), and 27% (PRIMA-PI). Pairwise concordance (patients allocated to the same risk category by two RS, Table 2) was lowest between IPI-FLIPI2, ILI-FLIPI2, and ILI-PRIMA-PI (51%), and highest between IPI-FLIPI (67%). All five RS predicted TTFT (P <0.01). Using logistic regression, all five RS predicted for the absence of complete response, as well as for POD24.
All five RS were predictive of PFS (P <0.0001), OS (P <0.0001, Figure), and LRD (P <0.001). Ten-year OS estimates for each high-risk group were as follows: 16% (IPI), 46% (ILI), 46% (FLIPI), 48% (FLIPI2), 43% (PRIMA-PI). Although PRIMA-PI identified a high-risk group (B2M >3 mg/L), no significant differences in OS were found according to bone marrow infiltration (pairwise P = 0.7). FLIPI was the only RS to predict HT, with 10-y cumulative incidences of 3%, 8% and 10% for low-, intermediate-, and high-risk patients, respectively (P = 0.04).
Conclusion
The five RS exhibit very subtle differences in their performance metrics. All of them predict TTFT, response, POD24, PFS, OS, and the risk of LRD. IPI identifies a small subset of patients with dismal outcomes. Bone marrow involvement did not impact OS, questioning the prognostic discrimination of the low- and intermediate-risk PRIMA-PI categories. In our series, FLIPI was the only RS to predict HT. In summary, all available RS are similarly valid for prognostication. Their potential to aid in the decision of initiating treatment should be explored.
Keyword(s): Follicular lymphoma, Prognostic groups, Survival prediction


