
Contributions
Abstract: PB1567
Type: Publication Only
Session title: Indolent and mantle-cell non-Hodgkin lymphoma - Clinical
Background
Although outcomes in follicular lymphoma (FL) are generally good, some patients experience early relapse or histological transformation (HT), which compromise their life expectancy. The Prognostic Nutritional Index (PNI), a parameter combining the serum albumin concentration and the absolute lymphocyte count, was initially designed to estimate the prognosis of patients undergoing gastrointestinal surgery, but it has then been successfully applied to a wide range of solid and hematological cancer types. This index, a putative combined measure of the nutritional and inflammatory status and host’s anti-tumor response, has not been well characterized in FL.
Aims
To evaluate the role of the PNI in a large single-center series of FL patients.
Methods
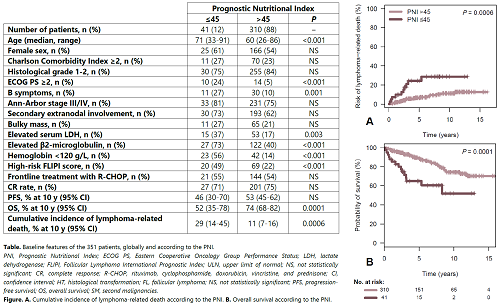
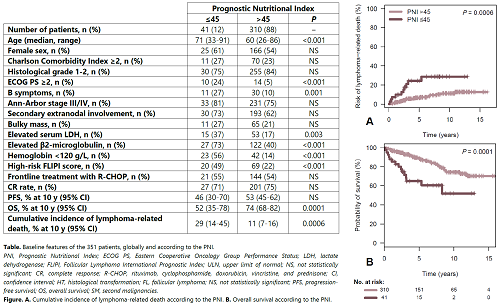
We studied 351 grade 1-3A FL patients (190 F / 160 M; median age, 61 years) diagnosed at a single institution between 2000 and 2018. The PNI (a unitless parameter) was calculated using the original formula (Buzby et al, Am J Surg, 1980): PNI = albumin (g/L) + [5 x absolute lymphocyte count (x109/L)]. Clinical characteristics, treatment modalities, response, progression-free (PFS) and overall survival (OS), risk of HT, and of second primary malignancies (SPM) were assessed and compared between patients with a PNI below and above 45, the most widespread cut-off.
Results
Forty-one patients (12%) had a PNI ≤45 (Table), who were older and showed adverse baseline features (poor ECOG PS, B symptoms, high LDH and/or β2-microglobulin levels, anemia, and high-risk FLIPI score). Median follow-up was 5 years (range, 0.8–16.2 years). Frontline treatment and responses were comparable among groups. Globally, PFS did not significantly differ based on the PNI. When a subgroup analysis was performed, a PNI ≤45 was predictive of a lower PFS in patients >60 years, but not in those ≤60 years. Using competing risks of death, the 10-year cumulative incidence of lymphoma-related death (progressive FL or treatment-related complications) was significantly higher for patients with a PNI ≤45 (29 vs. 11% at 10 years, P = 0.0006, Figure A). A low PNI was associated with a shorter OS in the global series (10-year OS, 52% versus 74%, P = 0.0001, Figure B). In a 6-element multivariate model also including the presence of B symptoms and of a bulky mass, ECOG PS, FLIPI score, and β2-microglobulin, the prognostic impact of the PNI on OS was confirmed for patients >60 years (HR = 3, P = 0.006). Finally, the PNI did not predict the risk of HT or SPM.
Conclusion
The PNI is a readily accessible piece of information that can identify a small subset of FL patients with shorter survival, especially among the older age subgroup. Upon validation in other series, it could be a valuable tool to anticipate outcomes and identify patients who could have their nutritional status optimized before treatment initiation.
Keyword(s): Follicular lymphoma, Prognostic factor, Survival prediction
Abstract: PB1567
Type: Publication Only
Session title: Indolent and mantle-cell non-Hodgkin lymphoma - Clinical
Background
Although outcomes in follicular lymphoma (FL) are generally good, some patients experience early relapse or histological transformation (HT), which compromise their life expectancy. The Prognostic Nutritional Index (PNI), a parameter combining the serum albumin concentration and the absolute lymphocyte count, was initially designed to estimate the prognosis of patients undergoing gastrointestinal surgery, but it has then been successfully applied to a wide range of solid and hematological cancer types. This index, a putative combined measure of the nutritional and inflammatory status and host’s anti-tumor response, has not been well characterized in FL.
Aims
To evaluate the role of the PNI in a large single-center series of FL patients.
Methods
We studied 351 grade 1-3A FL patients (190 F / 160 M; median age, 61 years) diagnosed at a single institution between 2000 and 2018. The PNI (a unitless parameter) was calculated using the original formula (Buzby et al, Am J Surg, 1980): PNI = albumin (g/L) + [5 x absolute lymphocyte count (x109/L)]. Clinical characteristics, treatment modalities, response, progression-free (PFS) and overall survival (OS), risk of HT, and of second primary malignancies (SPM) were assessed and compared between patients with a PNI below and above 45, the most widespread cut-off.
Results
Forty-one patients (12%) had a PNI ≤45 (Table), who were older and showed adverse baseline features (poor ECOG PS, B symptoms, high LDH and/or β2-microglobulin levels, anemia, and high-risk FLIPI score). Median follow-up was 5 years (range, 0.8–16.2 years). Frontline treatment and responses were comparable among groups. Globally, PFS did not significantly differ based on the PNI. When a subgroup analysis was performed, a PNI ≤45 was predictive of a lower PFS in patients >60 years, but not in those ≤60 years. Using competing risks of death, the 10-year cumulative incidence of lymphoma-related death (progressive FL or treatment-related complications) was significantly higher for patients with a PNI ≤45 (29 vs. 11% at 10 years, P = 0.0006, Figure A). A low PNI was associated with a shorter OS in the global series (10-year OS, 52% versus 74%, P = 0.0001, Figure B). In a 6-element multivariate model also including the presence of B symptoms and of a bulky mass, ECOG PS, FLIPI score, and β2-microglobulin, the prognostic impact of the PNI on OS was confirmed for patients >60 years (HR = 3, P = 0.006). Finally, the PNI did not predict the risk of HT or SPM.
Conclusion
The PNI is a readily accessible piece of information that can identify a small subset of FL patients with shorter survival, especially among the older age subgroup. Upon validation in other series, it could be a valuable tool to anticipate outcomes and identify patients who could have their nutritional status optimized before treatment initiation.
Keyword(s): Follicular lymphoma, Prognostic factor, Survival prediction


