
Contributions
Abstract: PB1505
Type: Publication Only
Session title: Chronic lymphocytic leukemia and related disorders - Clinical
Background
CLL (Chronic Lymphocytic Leukemia) activity is frequently manifested as anemia and/or thrombocytopenia, either as a result of bone marrow infiltration or autoimmunity, but CLL-related neutropenia is not common and it's effect on disease course is rarely reported. However, the development of neutropenia, especially when considering the underlying immune dysfunction of CLL patients, might contribute to infection risk and influence treatment decisions.
Aims
To study clinical characteristics, complications and treatment outcomes of CLL patients manifesting pre-treatment CLL-related neutropenia.
Methods
Cases were retrospectively collected from members of the Israeli CLL Study Group. Patients with a diagnosis of CLL/SLL (Small lymphocytic lymphoma) and neutropenia of < 1000/μL before initiating CLL directed therapy were included. Patients who developed neutropenia while receiving CLL directed therapy or following treatment were excluded.
Results
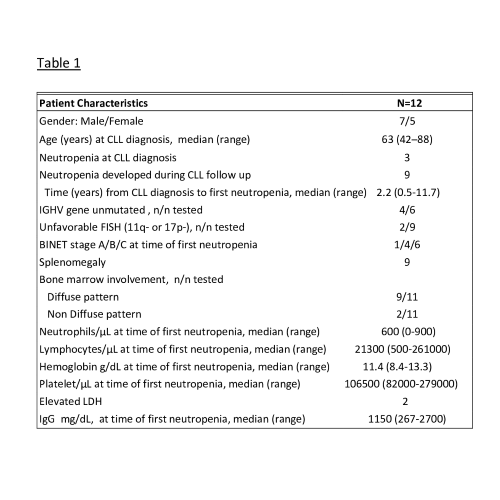
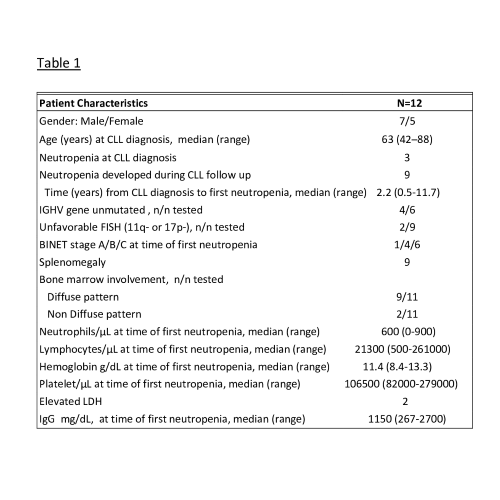
We identified 12 treatment-naïve CLL/SLL patients with neutropenia<1000/μL (CLL n=11, SLL n=1) (Table 1). Three patients presented with neutropenia concurrently with CLL/SLL diagnosis and nine developed neutropenia during CLL follow up, with median time of 2.2 years (0.5-11.7) post CLL diagnosis. Median neutrophils count at the time of first neutropenia was 600/μL (0-900). At the time of first neutropenia, six patients had isolated neutropenia without anemia or thrombocytopenia. Bone marrow biopsy was done in 11 patients, nine patients had diffuse infiltration pattern and two non- diffuse infiltration pattern. Nine patients had splenomegaly. Direct Coombs test was positive in six patients but no patient had clinically significant AIHA (Autoimmune hemolytic anemia) or ITP (Immune thrombocytopenia). Anti-neutrophils antibody test was done in one patient and was found negative. Low IgG level (<700 mg/dL) was present in four patients, low IgA (<70 mg/dL) in two and low IgM (<40 mg/dL) in five. Six treatment naive neutropenic patients developed Grade 3 or 4 infection (50% of the study cohort). The most common infection site was the skin and soft tissues (n=3), other infection sites include the oral cavity, gastrointestinal tract, urinary tract and lungs. Among the six patients with neutropenia and significant infection, four had low IgG levels. Supportive care with GCSF was administered in eight patients. Four patients received a course of steroids, concurrently with GCSF in three. CLL directed therapy was initiated in nine patients with median time from first neutropenia to CLL directed therapy of 104 days (Range, 6-490), eight patients received CLL-directed therapy within a year (Table 2). Treatment was chemoimmunotherapy in five patients, ibrutinib in two and venetoclax-obinutuzumab in two. Data on treatment toxicity is available for seven patients, among those- two patients developed neutropenic fever following cycle one of treatment and none had neutropenic fever during cycles 2-6 of treatment. Three patients on chemoimmunotherapy needed dose reduction due to treatment toxicity. No dose reduction was reported in patients on novel agents.
Conclusion
Neutropenia in treatment naïve CLL patients is accompanied by diffuse bone marrow involvement in most patients, although anemia and/or thrombocytopenia might be absent. Neutropenia can predispose patients to significant infections. Some patients will be managed solely with GSCF and/or steroids, but most patients will need CLL-directed therapy within a year.
Keyword(s): Chronic lymphocytic leukemia, Neutropenia
Abstract: PB1505
Type: Publication Only
Session title: Chronic lymphocytic leukemia and related disorders - Clinical
Background
CLL (Chronic Lymphocytic Leukemia) activity is frequently manifested as anemia and/or thrombocytopenia, either as a result of bone marrow infiltration or autoimmunity, but CLL-related neutropenia is not common and it's effect on disease course is rarely reported. However, the development of neutropenia, especially when considering the underlying immune dysfunction of CLL patients, might contribute to infection risk and influence treatment decisions.
Aims
To study clinical characteristics, complications and treatment outcomes of CLL patients manifesting pre-treatment CLL-related neutropenia.
Methods
Cases were retrospectively collected from members of the Israeli CLL Study Group. Patients with a diagnosis of CLL/SLL (Small lymphocytic lymphoma) and neutropenia of < 1000/μL before initiating CLL directed therapy were included. Patients who developed neutropenia while receiving CLL directed therapy or following treatment were excluded.
Results
We identified 12 treatment-naïve CLL/SLL patients with neutropenia<1000/μL (CLL n=11, SLL n=1) (Table 1). Three patients presented with neutropenia concurrently with CLL/SLL diagnosis and nine developed neutropenia during CLL follow up, with median time of 2.2 years (0.5-11.7) post CLL diagnosis. Median neutrophils count at the time of first neutropenia was 600/μL (0-900). At the time of first neutropenia, six patients had isolated neutropenia without anemia or thrombocytopenia. Bone marrow biopsy was done in 11 patients, nine patients had diffuse infiltration pattern and two non- diffuse infiltration pattern. Nine patients had splenomegaly. Direct Coombs test was positive in six patients but no patient had clinically significant AIHA (Autoimmune hemolytic anemia) or ITP (Immune thrombocytopenia). Anti-neutrophils antibody test was done in one patient and was found negative. Low IgG level (<700 mg/dL) was present in four patients, low IgA (<70 mg/dL) in two and low IgM (<40 mg/dL) in five. Six treatment naive neutropenic patients developed Grade 3 or 4 infection (50% of the study cohort). The most common infection site was the skin and soft tissues (n=3), other infection sites include the oral cavity, gastrointestinal tract, urinary tract and lungs. Among the six patients with neutropenia and significant infection, four had low IgG levels. Supportive care with GCSF was administered in eight patients. Four patients received a course of steroids, concurrently with GCSF in three. CLL directed therapy was initiated in nine patients with median time from first neutropenia to CLL directed therapy of 104 days (Range, 6-490), eight patients received CLL-directed therapy within a year (Table 2). Treatment was chemoimmunotherapy in five patients, ibrutinib in two and venetoclax-obinutuzumab in two. Data on treatment toxicity is available for seven patients, among those- two patients developed neutropenic fever following cycle one of treatment and none had neutropenic fever during cycles 2-6 of treatment. Three patients on chemoimmunotherapy needed dose reduction due to treatment toxicity. No dose reduction was reported in patients on novel agents.
Conclusion
Neutropenia in treatment naïve CLL patients is accompanied by diffuse bone marrow involvement in most patients, although anemia and/or thrombocytopenia might be absent. Neutropenia can predispose patients to significant infections. Some patients will be managed solely with GSCF and/or steroids, but most patients will need CLL-directed therapy within a year.
Keyword(s): Chronic lymphocytic leukemia, Neutropenia


