
Contributions
Abstract: PB1497
Type: Publication Only
Session title: Chronic lymphocytic leukemia and related disorders - Clinical
Background
Clinical course of CLL is heterogeneous and asymptomatic patients with early stage should receive active surveillance until there is evidence for progression. Several molecular, genetic and clinical prognostic markers were demonstrated to be capable of predicting the probability of treatment and various prognostic models have been proposed to predict time to first treatment (TTFT).
Aims
To explored the potency of four proposed models (IPS-E, CLL-IPI, CLL1-PM and Barcelona-Brno prognostic model) to predict TTFT using our Han cohort. All four models were initially based on western population. Considering the significant difference of CLL between Western and Asian population, the models should be validated and discussed thoroughly among all ethnics prior to its broader implementation.
Methods
From the database of Department of Hematology and Pukou CLL Center, The First Affiliated Hospital of Nanjing Medical University, a total of 110 newly diagnosed Binet stage A CLL patients without indication for treatment from Jun, 2009 and to Jan, 2020 were enrolled in our cohort. The diagnosis of CLL and stage of disease was strictly in line with the updated guidelines from iwCLL. All included patients underwent active survelliance as initial management, defined as no treatment need within the first 3 months after diagnosis and patients who didn’t meet the indication for treatment were censored at date of statistical analysis. The endpoint was TTFT, which was defined as the time interval between diagnosis and start of treatment due to disease progression. We collected all parameters at diagnosis as mentioned in previous four prognostic models: (1) clinical manifestation (age, Binet and Rai stage and lymph nodes size); (2) absolute lymphocyte count (ALC) and lymphocyte doubling time (LDT); (3) b2-Microglobulin (β2‐MG); (4) del [17p], del [11q] analyzed by FISH; (5) IGHV mutation status.
Results
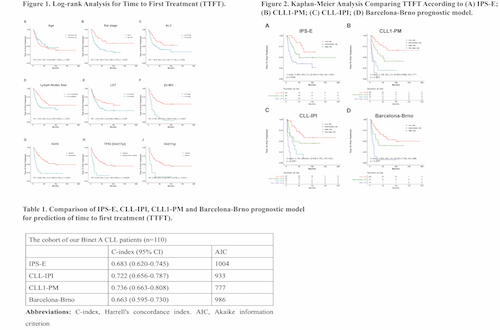
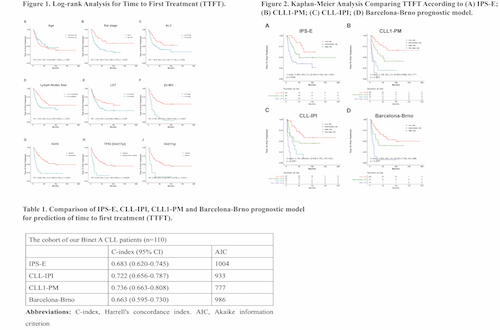
110 asymptomatic Binet A patients were included in our study; the median age was 58 years old (25-84). The median follow-up time was 35 months (4-189 months), 57 patients (51.8%) met the indication for treatment due to disease symptomatic progression during follow-up. Log-rank test was performed to analyze the independent risk factors associated with TTFT. Seven variables were found to be independently associated with TTFT including Rai stage, ALC > 15×109/L, palpable lymph node ≥ 1 cm, β2-MG > 3.5 mg/L, unmutated IGHV, TP53 disruption and 11q deletion (Figure 1). However, age older than 60 years old and LDT<12 months, as proposed in CLL1-PM model, failed to show correlation with shorter TTFT (p=0.383 and p=0.087, respectively) in our cohort. Stratification of patients according to IPS-E, CLL-IPI, CLL1-PM and Barcelona-Brno prognostic model all showed significant difference in terms of TTFT (Figure 2). The predictive power of four prognostic models was further assessed by Harrell’s C-index and AIC. C-index was highest in CLL1-PM, followed by CLL-IPI, IPS-E and Barcelona-Brno prognostic model. The AIC values were lowest in CLL1-PM, followed by CLL-IPI, Barcelona-Brno and IPS-E (Table 1).
Conclusion
All four prognostic models had their efficacy in prediction of TTFT. IPS-E might be an ideal model for patients who undergo basic clinical examination so that fundamental evaluation could be conducted to guide clinical surveillance. For patients yearn for active assessment, FISH and NGS were recommended and CLL-IPI could be used to predict their prognosis more accurately and comprehensively.
Keyword(s): Chronic lymphocytic leukemia, Prognosis
Abstract: PB1497
Type: Publication Only
Session title: Chronic lymphocytic leukemia and related disorders - Clinical
Background
Clinical course of CLL is heterogeneous and asymptomatic patients with early stage should receive active surveillance until there is evidence for progression. Several molecular, genetic and clinical prognostic markers were demonstrated to be capable of predicting the probability of treatment and various prognostic models have been proposed to predict time to first treatment (TTFT).
Aims
To explored the potency of four proposed models (IPS-E, CLL-IPI, CLL1-PM and Barcelona-Brno prognostic model) to predict TTFT using our Han cohort. All four models were initially based on western population. Considering the significant difference of CLL between Western and Asian population, the models should be validated and discussed thoroughly among all ethnics prior to its broader implementation.
Methods
From the database of Department of Hematology and Pukou CLL Center, The First Affiliated Hospital of Nanjing Medical University, a total of 110 newly diagnosed Binet stage A CLL patients without indication for treatment from Jun, 2009 and to Jan, 2020 were enrolled in our cohort. The diagnosis of CLL and stage of disease was strictly in line with the updated guidelines from iwCLL. All included patients underwent active survelliance as initial management, defined as no treatment need within the first 3 months after diagnosis and patients who didn’t meet the indication for treatment were censored at date of statistical analysis. The endpoint was TTFT, which was defined as the time interval between diagnosis and start of treatment due to disease progression. We collected all parameters at diagnosis as mentioned in previous four prognostic models: (1) clinical manifestation (age, Binet and Rai stage and lymph nodes size); (2) absolute lymphocyte count (ALC) and lymphocyte doubling time (LDT); (3) b2-Microglobulin (β2‐MG); (4) del [17p], del [11q] analyzed by FISH; (5) IGHV mutation status.
Results
110 asymptomatic Binet A patients were included in our study; the median age was 58 years old (25-84). The median follow-up time was 35 months (4-189 months), 57 patients (51.8%) met the indication for treatment due to disease symptomatic progression during follow-up. Log-rank test was performed to analyze the independent risk factors associated with TTFT. Seven variables were found to be independently associated with TTFT including Rai stage, ALC > 15×109/L, palpable lymph node ≥ 1 cm, β2-MG > 3.5 mg/L, unmutated IGHV, TP53 disruption and 11q deletion (Figure 1). However, age older than 60 years old and LDT<12 months, as proposed in CLL1-PM model, failed to show correlation with shorter TTFT (p=0.383 and p=0.087, respectively) in our cohort. Stratification of patients according to IPS-E, CLL-IPI, CLL1-PM and Barcelona-Brno prognostic model all showed significant difference in terms of TTFT (Figure 2). The predictive power of four prognostic models was further assessed by Harrell’s C-index and AIC. C-index was highest in CLL1-PM, followed by CLL-IPI, IPS-E and Barcelona-Brno prognostic model. The AIC values were lowest in CLL1-PM, followed by CLL-IPI, Barcelona-Brno and IPS-E (Table 1).
Conclusion
All four prognostic models had their efficacy in prediction of TTFT. IPS-E might be an ideal model for patients who undergo basic clinical examination so that fundamental evaluation could be conducted to guide clinical surveillance. For patients yearn for active assessment, FISH and NGS were recommended and CLL-IPI could be used to predict their prognosis more accurately and comprehensively.
Keyword(s): Chronic lymphocytic leukemia, Prognosis


