
Contributions
Abstract: PB1495
Type: Publication Only
Session title: Chronic lymphocytic leukemia and related disorders - Clinical
Background
Chronic lymphocytic leukemia (CLL) is a pathology with a variable clinical evolution; some patients remain indolent for many years while others require treatment, including shortly after diagnosis. Although molecular and genetic markers with prognostic value have been described, the current International Workshop on Chronic Lymphocytic Leukemia (iwCLL) guidelines only recommends their analysis prior to commencing treatment.
Aims
In this retrospective study, we analyzed the prognostic impact of molecular and genetic markers on CLL patients at diagnosis.
Methods
A consecutive series of 217 patients with CLL diagnosed in our hospital between 2008 and 2018 was analyzed. Clinical, molecular (IGHV and TP53) and cytogenetic data were collected at diagnosis.
Results
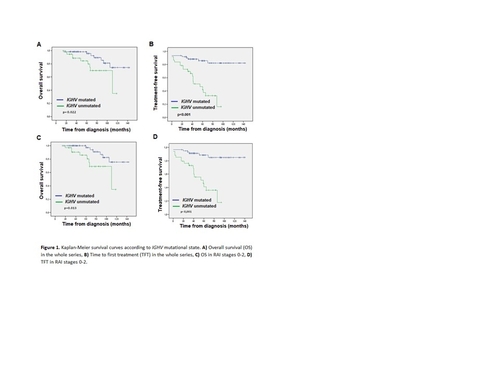
Our series confirmed the prognostic value of the CLL-IPI index for OS (p=0.003, Log-Rank test) and time to first treatment (TFT, p<0.001). In accordance with previously published results, Kaplan-Meier survival analyses identified an association between IGHV unmutated (p<0.022) (Figure 1A and 1B) and shorter OS and TFT (p≤0.001). The variables age >65 years (p<0.001), β2-microglobulin >3.5 mg/dL (p<0.001) and advanced Binet/Rai clinical stage (p=0.001) were also associated with shorter OS and TFT, while the presence of mutation/deletion of TP53 (p=0.001) and deletion of 11q (p<0.001) were associated with shorter TFT. Unmutated IGHV, advanced clinical stage and age (albeit marginally) also showed independent prognostic value for OS as determined by multivariate analysis (Table 1, p=0.01, 0.033, and 0.072 respectively). For TFT, only unmutated IGHV and clinical stage (albeit marginally) had prognostic impact (p=0.001 and 0.081, respectively).
|
| OS | TFT | |||||
Group | Variable | p-value | HR | 95% CI | p-value | HR | 95% CI | |
Whole series | B2MG | >3.5 mg/L | 0.729 | 0.73 | 0.12–4.30 | 0.421 | 1.75 | 0.45–6.89 |
IGHV | Unmutated | 0.01 | 6.16 | 1.56–24.37 | 0.001 | 13.58 | 2.91–63.29 | |
Age | >65 years | 0.072 | 3.57 | 0.89–14.31 |
| |||
RAI | 3-4 | 0.033 | 27.22 | 1.30–572.00 | 0.081 | 9.67 | 0.76–123.70 | |
Table 1. Multivariate analysis of overall survival (OS) and time to first treatment (TFT).
Importantly, when only patients in the early stages were selected (RAI 0-2/BINET A), IGHV mutation maintained prognostic value for both OS and TFT in the multivariate analysis (OS: OR 6.16, p=0.01/OR 5.96, p=0.009; TFT: OR 13.58, p=0.001/OR 14.08, p=0.001) and Kaplan-Meier survival analyses (OS: p=0.013, TFT: p<0.001) (Figure 1C and 1D). The loss of prognostic value of β2-microglobulin levels might be explained by the statistically significant association observed in our series between unmutated IGHV and β2-microglobulin levels > 3.5 mg/dL (p = 0.002, Pearson’s χ2) as well as advanced age (p = 0.024, Pearson’s χ2). Chromosomal alterations, such as deletion/mutation of TP53 and deletion of 11q, were not included in the multivariate analysis due to their low incidence in our series. A larger series would be required to evaluate their prognostic impact.
Conclusion
IGHV mutational state was the only prognostic marker to have independent prognostic value for both OS and TFT, for the whole series as well as patients in the early stages. Our results indicate that the determination of IGHV mutational state at diagnosis informs the risk stratification of patients with CLL.
Keyword(s): IgH rearrangment, Molecular markers, Prognosis
Abstract: PB1495
Type: Publication Only
Session title: Chronic lymphocytic leukemia and related disorders - Clinical
Background
Chronic lymphocytic leukemia (CLL) is a pathology with a variable clinical evolution; some patients remain indolent for many years while others require treatment, including shortly after diagnosis. Although molecular and genetic markers with prognostic value have been described, the current International Workshop on Chronic Lymphocytic Leukemia (iwCLL) guidelines only recommends their analysis prior to commencing treatment.
Aims
In this retrospective study, we analyzed the prognostic impact of molecular and genetic markers on CLL patients at diagnosis.
Methods
A consecutive series of 217 patients with CLL diagnosed in our hospital between 2008 and 2018 was analyzed. Clinical, molecular (IGHV and TP53) and cytogenetic data were collected at diagnosis.
Results
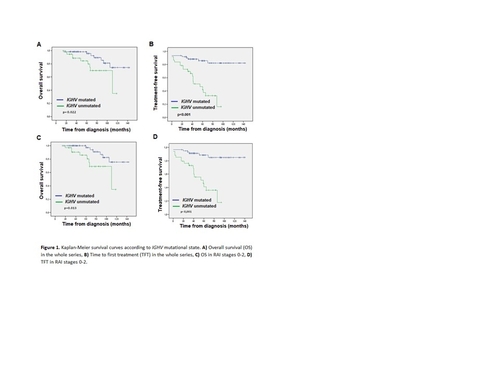
Our series confirmed the prognostic value of the CLL-IPI index for OS (p=0.003, Log-Rank test) and time to first treatment (TFT, p<0.001). In accordance with previously published results, Kaplan-Meier survival analyses identified an association between IGHV unmutated (p<0.022) (Figure 1A and 1B) and shorter OS and TFT (p≤0.001). The variables age >65 years (p<0.001), β2-microglobulin >3.5 mg/dL (p<0.001) and advanced Binet/Rai clinical stage (p=0.001) were also associated with shorter OS and TFT, while the presence of mutation/deletion of TP53 (p=0.001) and deletion of 11q (p<0.001) were associated with shorter TFT. Unmutated IGHV, advanced clinical stage and age (albeit marginally) also showed independent prognostic value for OS as determined by multivariate analysis (Table 1, p=0.01, 0.033, and 0.072 respectively). For TFT, only unmutated IGHV and clinical stage (albeit marginally) had prognostic impact (p=0.001 and 0.081, respectively).
|
| OS | TFT | |||||
Group | Variable | p-value | HR | 95% CI | p-value | HR | 95% CI | |
Whole series | B2MG | >3.5 mg/L | 0.729 | 0.73 | 0.12–4.30 | 0.421 | 1.75 | 0.45–6.89 |
IGHV | Unmutated | 0.01 | 6.16 | 1.56–24.37 | 0.001 | 13.58 | 2.91–63.29 | |
Age | >65 years | 0.072 | 3.57 | 0.89–14.31 |
| |||
RAI | 3-4 | 0.033 | 27.22 | 1.30–572.00 | 0.081 | 9.67 | 0.76–123.70 | |
Table 1. Multivariate analysis of overall survival (OS) and time to first treatment (TFT).
Importantly, when only patients in the early stages were selected (RAI 0-2/BINET A), IGHV mutation maintained prognostic value for both OS and TFT in the multivariate analysis (OS: OR 6.16, p=0.01/OR 5.96, p=0.009; TFT: OR 13.58, p=0.001/OR 14.08, p=0.001) and Kaplan-Meier survival analyses (OS: p=0.013, TFT: p<0.001) (Figure 1C and 1D). The loss of prognostic value of β2-microglobulin levels might be explained by the statistically significant association observed in our series between unmutated IGHV and β2-microglobulin levels > 3.5 mg/dL (p = 0.002, Pearson’s χ2) as well as advanced age (p = 0.024, Pearson’s χ2). Chromosomal alterations, such as deletion/mutation of TP53 and deletion of 11q, were not included in the multivariate analysis due to their low incidence in our series. A larger series would be required to evaluate their prognostic impact.
Conclusion
IGHV mutational state was the only prognostic marker to have independent prognostic value for both OS and TFT, for the whole series as well as patients in the early stages. Our results indicate that the determination of IGHV mutational state at diagnosis informs the risk stratification of patients with CLL.
Keyword(s): IgH rearrangment, Molecular markers, Prognosis


