
Contributions
Abstract: PB1479
Type: Publication Only
Session title: Bone marrow failure syndromes incl. PNH - Clinical
Background
The most common symptoms seen in COVID-19 patients are fever, fatigue, and dry cough, and dyspnea. Although there is comparatively few rising reports on the hematological sequelae. Hematological changes commonly described in patients with COVID-19, include reduced lymphocyte count and platelet count but normal white blood cell count. we present a case of pancytopenia and hypocellular marrow which is not a commonly known sequalae of COVID 19 infection.
Aims
To describe a novel case of coronavirus disease 2019 (COVID-19)-associated aplastic anemia in a patient known to have primary glomerulonephritis.
Methods
we described a case report of hematological sequalae of a COVID 19 case including the clinical presentation, management, and response to therapy
Results
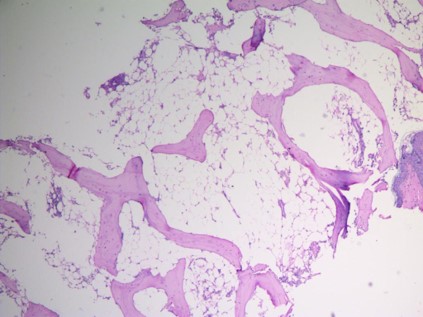
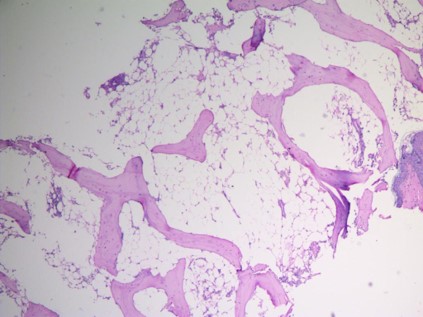
A 25-year-old lady with a background of primary membranous glomerulonephritis with crescent formation required therapy with rituximab monoclonal anti CD20, presented with anemia, mucocutaneous bleeding. 25 days before her presentation she had subjective fever, cough, and dyspnea with radiological findings highly suspicious for COVID 19 and she tested positive for COVID-19 by PCR on nasopharyngeal swab. Isolation at home was recommended for her as she had mild-moderate COVID19 and her swab turned negative after 15 days of onset of the respiratory symptoms. she experienced pallor and muco-cutaneous bleeding in form of ecchymosis all over the body, wet purpura but the rest of her clinical examination was free, her CBC revealed hemoglobin: 6.9 g/dl; WBC: 2.67×103/mm3; platelets: 10×103/mm3. MCV 79 with reticulocytopenia, all immunological profiles as well as virology screening for HCV, HBV, HIV, CMV and EBV were negative. Bone marrow aspirate and biopsy revealed marked hypocellular marrow (cellularity 20%) with all bone marrow element were markedly depressed. Cyclosporine was prescribed for her as well as eltrombopag in the dose of 50 mg/day orally which titrated gradually according to platelet response to 100 mg/day PO with repeated irradiated packed RBCs and platelet transfusion during hospital stay.
During her hospital stay her liver enzymes (AST & ALT) were elevated so doses of cyclosporine and eltrombopag were decreased till the normalization of her liver enzymes then reiterated again according to the hematological response. She is maintained on this protocol now for 2 months with minimal hematological response. she prepared now for HLA matching and hematopoietic stem cell transplantation.
Conclusion
Further exploration of potential COVID-19-related hematological abnormalities is needed and requires extensive collaboration to collect large, organized data sets. The possibility of an immune-mediated process and its therapeutic implications also warrants greater study.
Keyword(s): Aplastic anemia, COVID-19
Abstract: PB1479
Type: Publication Only
Session title: Bone marrow failure syndromes incl. PNH - Clinical
Background
The most common symptoms seen in COVID-19 patients are fever, fatigue, and dry cough, and dyspnea. Although there is comparatively few rising reports on the hematological sequelae. Hematological changes commonly described in patients with COVID-19, include reduced lymphocyte count and platelet count but normal white blood cell count. we present a case of pancytopenia and hypocellular marrow which is not a commonly known sequalae of COVID 19 infection.
Aims
To describe a novel case of coronavirus disease 2019 (COVID-19)-associated aplastic anemia in a patient known to have primary glomerulonephritis.
Methods
we described a case report of hematological sequalae of a COVID 19 case including the clinical presentation, management, and response to therapy
Results
A 25-year-old lady with a background of primary membranous glomerulonephritis with crescent formation required therapy with rituximab monoclonal anti CD20, presented with anemia, mucocutaneous bleeding. 25 days before her presentation she had subjective fever, cough, and dyspnea with radiological findings highly suspicious for COVID 19 and she tested positive for COVID-19 by PCR on nasopharyngeal swab. Isolation at home was recommended for her as she had mild-moderate COVID19 and her swab turned negative after 15 days of onset of the respiratory symptoms. she experienced pallor and muco-cutaneous bleeding in form of ecchymosis all over the body, wet purpura but the rest of her clinical examination was free, her CBC revealed hemoglobin: 6.9 g/dl; WBC: 2.67×103/mm3; platelets: 10×103/mm3. MCV 79 with reticulocytopenia, all immunological profiles as well as virology screening for HCV, HBV, HIV, CMV and EBV were negative. Bone marrow aspirate and biopsy revealed marked hypocellular marrow (cellularity 20%) with all bone marrow element were markedly depressed. Cyclosporine was prescribed for her as well as eltrombopag in the dose of 50 mg/day orally which titrated gradually according to platelet response to 100 mg/day PO with repeated irradiated packed RBCs and platelet transfusion during hospital stay.
During her hospital stay her liver enzymes (AST & ALT) were elevated so doses of cyclosporine and eltrombopag were decreased till the normalization of her liver enzymes then reiterated again according to the hematological response. She is maintained on this protocol now for 2 months with minimal hematological response. she prepared now for HLA matching and hematopoietic stem cell transplantation.
Conclusion
Further exploration of potential COVID-19-related hematological abnormalities is needed and requires extensive collaboration to collect large, organized data sets. The possibility of an immune-mediated process and its therapeutic implications also warrants greater study.
Keyword(s): Aplastic anemia, COVID-19


