Contributions
Abstract: PB1405
Type: Publication Only
Session title: Acute myeloid leukemia - Clinical
Background
There is a range of estimates for the frequency of FMS-like tyrosine kinase 3 (FLT3) mutations in patients with acute myeloid leukemia (AML) in the literature, but no available systematic review on this topic.
Aims
To provide a comprehensive review of the FLT3 mutation frequency in unselected populations of patients with AML.
Methods
We conducted systematic literature searches of the Medline/PubMed and Embase databases through 31/08/2020. Search terms were “acute myeloid leukemia,” “AML,” “fms like tyrosine kinase 3,” and “FLT3” combined with “epidemiology,” “incidence,” “prevalence,” “frequency,” “presentation,” and “occurrence.” There were no limits on publication year. Full-text English-language papers of studies with ≥200 total patients were selected. Only studies reporting data for both the FLT3–internal tandem duplication (FLT3-ITD) mutation and FLT3–tyrosine kinase domain (FLT3-TKD) point mutation, study location (country), population source (eg, hospital or medical center), data collection dates, age range, sex distribution, and a description of FLT3 mutation test methodology were included. Animal studies, in vitro studies, case reports, commentaries, reviews, and clinical trials were excluded. Using meta-analysis methods, weighted summary estimates and confidence intervals (CIs) were generated for each FLT3 mutation from untransformed data.
Results
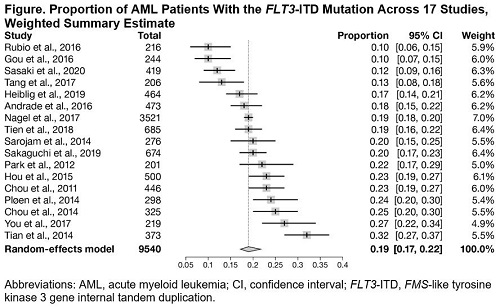
Of 1,618 records identified, 17 studies were included (16 hospital or medical center cohort studies, one cross-sectional study). Studies were conducted in Asia, Europe, South America, or North America with data collection dates ranging from 1994 through 2018. Sample sizes for the 16 cohort studies ranged from 201 to 685 total patients; the cross-sectional study included 3,521 patients. Across studies, 46.8% to 60.0% of participants were male. One study included only children (aged 0-17.9 years [Rubio 2016]), two studies included children and adults (aged 1-84 years [You 2017]; 0-21 years [median: 7 years] [Andrade 2016]), and 14 studies included patients aged ≥15 years. All studies reported using a polymerase chain reaction (PCR)–based test to identify the mutations; some studies reported also using additional methods (gene sequencing, fluorescence fragment analysis). Across the 17 studies, the frequency of FLT3-ITD mutation ranged from 10.2% to 31.6% (Figure), and the frequency of FLT3-TKD mutation ranged from 1.9% to 8.8% (not shown). These ranges were unchanged when the three studies with patients aged <15 years were excluded. Due to heterogeneity in study results, random-effects models were chosen, with weighted summary estimates of 19% (95% CI: 17%-22%) for a FLT3-ITD mutation and 5% (95% CI: 4%-6%) for a FLT3-TKD mutation. Weighted summary estimates were similar using fixed-effects models and when data were transformed (Freeman-Tukey double arcsine transformation). There was no obvious association across studies between FLT3-ITD frequency and FLT3-TKD frequency, or between FLT3 mutation frequency and age, geographical setting, or population source.
Conclusion
We conducted a comprehensive systematic review of the frequency of the FLT3 mutation in unselected populations of patients with AML. The results suggest a population frequency of around 19% for a FLT3-ITD mutation and 5% for a FLT3-TKD mutation. Further research is needed to help explain the heterogeneity in the frequency of the FLT3 mutation across populations, and to put these results into context (including comparison with selected populations, such as in clinical trials).
Keyword(s): FLT3, Flt3-ITD, Meta-analysis, Mutation status
Abstract: PB1405
Type: Publication Only
Session title: Acute myeloid leukemia - Clinical
Background
There is a range of estimates for the frequency of FMS-like tyrosine kinase 3 (FLT3) mutations in patients with acute myeloid leukemia (AML) in the literature, but no available systematic review on this topic.
Aims
To provide a comprehensive review of the FLT3 mutation frequency in unselected populations of patients with AML.
Methods
We conducted systematic literature searches of the Medline/PubMed and Embase databases through 31/08/2020. Search terms were “acute myeloid leukemia,” “AML,” “fms like tyrosine kinase 3,” and “FLT3” combined with “epidemiology,” “incidence,” “prevalence,” “frequency,” “presentation,” and “occurrence.” There were no limits on publication year. Full-text English-language papers of studies with ≥200 total patients were selected. Only studies reporting data for both the FLT3–internal tandem duplication (FLT3-ITD) mutation and FLT3–tyrosine kinase domain (FLT3-TKD) point mutation, study location (country), population source (eg, hospital or medical center), data collection dates, age range, sex distribution, and a description of FLT3 mutation test methodology were included. Animal studies, in vitro studies, case reports, commentaries, reviews, and clinical trials were excluded. Using meta-analysis methods, weighted summary estimates and confidence intervals (CIs) were generated for each FLT3 mutation from untransformed data.
Results
Of 1,618 records identified, 17 studies were included (16 hospital or medical center cohort studies, one cross-sectional study). Studies were conducted in Asia, Europe, South America, or North America with data collection dates ranging from 1994 through 2018. Sample sizes for the 16 cohort studies ranged from 201 to 685 total patients; the cross-sectional study included 3,521 patients. Across studies, 46.8% to 60.0% of participants were male. One study included only children (aged 0-17.9 years [Rubio 2016]), two studies included children and adults (aged 1-84 years [You 2017]; 0-21 years [median: 7 years] [Andrade 2016]), and 14 studies included patients aged ≥15 years. All studies reported using a polymerase chain reaction (PCR)–based test to identify the mutations; some studies reported also using additional methods (gene sequencing, fluorescence fragment analysis). Across the 17 studies, the frequency of FLT3-ITD mutation ranged from 10.2% to 31.6% (Figure), and the frequency of FLT3-TKD mutation ranged from 1.9% to 8.8% (not shown). These ranges were unchanged when the three studies with patients aged <15 years were excluded. Due to heterogeneity in study results, random-effects models were chosen, with weighted summary estimates of 19% (95% CI: 17%-22%) for a FLT3-ITD mutation and 5% (95% CI: 4%-6%) for a FLT3-TKD mutation. Weighted summary estimates were similar using fixed-effects models and when data were transformed (Freeman-Tukey double arcsine transformation). There was no obvious association across studies between FLT3-ITD frequency and FLT3-TKD frequency, or between FLT3 mutation frequency and age, geographical setting, or population source.
Conclusion
We conducted a comprehensive systematic review of the frequency of the FLT3 mutation in unselected populations of patients with AML. The results suggest a population frequency of around 19% for a FLT3-ITD mutation and 5% for a FLT3-TKD mutation. Further research is needed to help explain the heterogeneity in the frequency of the FLT3 mutation across populations, and to put these results into context (including comparison with selected populations, such as in clinical trials).
Keyword(s): FLT3, Flt3-ITD, Meta-analysis, Mutation status