
Contributions
Abstract: PB1396
Type: Publication Only
Session title: Acute myeloid leukemia - Clinical
Background
Acute myeloid leukemia with t(8;21)(q22;q22.1) translocation was classified as favorable risk group in NCCN guidelines, whereas KIT D816mutations is a poor prognostic factor. Such patients with concurrent systemic mastocytosis are extremely rare, their clinical features and prognosis are still unclear.
Aims
To explore the clinical features and prognosis of t(8;21)AML bearing KIT D816 mutation associated with SM.
Methods
The clinical data, outcomes of chemotherapy and allo-HSCT of 5 patients with t(8;21) AML bearing KIT D816 mutation associated with SM admitted to Hebei Yanda Ludaopei Hospital from July 3, 2019 to February 1, 2021 were retrospectively analyzed. The median follow-up time was 323 (112-580) days.
Results
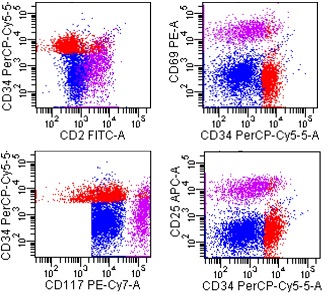
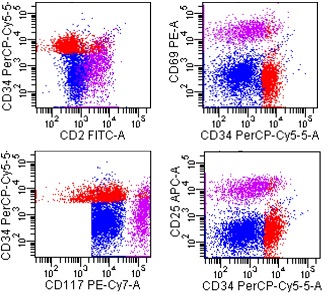
Among the 5 patients, 4 were males and 1 female, with a median age of 9 (3-16) years old. The median ratio of bone marrow blasts at onset was 64 (46-78.5)%; the chromosome was t(8;21)(q22;q22.1), and the RUNX1-RUNX1T1 fusion gene was positive. After 2 courses of chemotherapy, 3 patients achieved complete morphological remission, and 2 patients were in NR status. Flow cytometry shows malignant myeloblasts in 3 patients, in addition abnormal mast cells were found in 4 patients. A less than 3log reduction of RUNX1/RUNX1T1 transcript in bone marrow was seen in all of 5 patients. The flow sorting of 2 patients showed that the RUNX1-RUNX1T1 fusion gene mainly been expressed by abnormal mast cell. 4 patients underwent allo-HSCT, all haplotype 5/10 compatible, adopting Bu/Cy-based myeloablative intensified conditioning regimen. After transplantation, all 4 patients had hematopoietic engraftment. The bone marrow findings at +30 days all showed CR status, no malignant myeloblasts were found in bone marrow flow cytometry, yet abnormal phenotypic mast cells were found. RUNX1-RUNX1T1 transcripts did not turn negative. All 5 patients met the diagnostic criteria for SM: ① KIT D816 mutation was detected (3 cases of D816V mutation, 3 cases of D816Y mutation, 1 case of D816F mutation; 1 patient had the above 3 mutations); ②>25% of mast cells found in bone marrow cytology of all patients were immature or atypical mast cells; ③mast cells all expressed CD25, with or without CD2. Subsequently 1 patients was treated with midostaurin, RUNX1-RUNX1T1 and mast cells became negative after 63 days of treatment. The other 3 patients were treated with dasatinib and/or interferon. The fusion genes and abnormal mast cells did not turn negative. Patient who did not undergo transplantation continued to detect abnormal mast cells and transcripts of RUNX1-RUNX1T1.
Conclusion
t(8;21)AML bearing KIT D816 mutation associated with SM shows poor response to common chemotherapy and allo-HSCT, neither can eliminate clonal mast cells, hence this type of disease requires targeted therapy intervention.
Keyword(s): Acute myeloid leukemia, Kit, RUNX1, Systemic mastocytosis
Abstract: PB1396
Type: Publication Only
Session title: Acute myeloid leukemia - Clinical
Background
Acute myeloid leukemia with t(8;21)(q22;q22.1) translocation was classified as favorable risk group in NCCN guidelines, whereas KIT D816mutations is a poor prognostic factor. Such patients with concurrent systemic mastocytosis are extremely rare, their clinical features and prognosis are still unclear.
Aims
To explore the clinical features and prognosis of t(8;21)AML bearing KIT D816 mutation associated with SM.
Methods
The clinical data, outcomes of chemotherapy and allo-HSCT of 5 patients with t(8;21) AML bearing KIT D816 mutation associated with SM admitted to Hebei Yanda Ludaopei Hospital from July 3, 2019 to February 1, 2021 were retrospectively analyzed. The median follow-up time was 323 (112-580) days.
Results
Among the 5 patients, 4 were males and 1 female, with a median age of 9 (3-16) years old. The median ratio of bone marrow blasts at onset was 64 (46-78.5)%; the chromosome was t(8;21)(q22;q22.1), and the RUNX1-RUNX1T1 fusion gene was positive. After 2 courses of chemotherapy, 3 patients achieved complete morphological remission, and 2 patients were in NR status. Flow cytometry shows malignant myeloblasts in 3 patients, in addition abnormal mast cells were found in 4 patients. A less than 3log reduction of RUNX1/RUNX1T1 transcript in bone marrow was seen in all of 5 patients. The flow sorting of 2 patients showed that the RUNX1-RUNX1T1 fusion gene mainly been expressed by abnormal mast cell. 4 patients underwent allo-HSCT, all haplotype 5/10 compatible, adopting Bu/Cy-based myeloablative intensified conditioning regimen. After transplantation, all 4 patients had hematopoietic engraftment. The bone marrow findings at +30 days all showed CR status, no malignant myeloblasts were found in bone marrow flow cytometry, yet abnormal phenotypic mast cells were found. RUNX1-RUNX1T1 transcripts did not turn negative. All 5 patients met the diagnostic criteria for SM: ① KIT D816 mutation was detected (3 cases of D816V mutation, 3 cases of D816Y mutation, 1 case of D816F mutation; 1 patient had the above 3 mutations); ②>25% of mast cells found in bone marrow cytology of all patients were immature or atypical mast cells; ③mast cells all expressed CD25, with or without CD2. Subsequently 1 patients was treated with midostaurin, RUNX1-RUNX1T1 and mast cells became negative after 63 days of treatment. The other 3 patients were treated with dasatinib and/or interferon. The fusion genes and abnormal mast cells did not turn negative. Patient who did not undergo transplantation continued to detect abnormal mast cells and transcripts of RUNX1-RUNX1T1.
Conclusion
t(8;21)AML bearing KIT D816 mutation associated with SM shows poor response to common chemotherapy and allo-HSCT, neither can eliminate clonal mast cells, hence this type of disease requires targeted therapy intervention.
Keyword(s): Acute myeloid leukemia, Kit, RUNX1, Systemic mastocytosis


