
Contributions
Abstract: PB1392
Type: Publication Only
Session title: Acute myeloid leukemia - Clinical
Background
Acute Myeloid Leukemia (AML) is a bone marrow clonal disorder characterized by the proliferation of myeloid blasts. The European LeukemiaNet (ELN) 2017 risk stratification is a consolidated prognostic system focused on AML genetic features which is able to predict the probability of AML response and relapse following an intensive chemotherapeutic approach.
However, chemosensitivity and risk of disease relapse is age-dependent and limited for patient aged up to 60 years.
Aims
We investigated the predictability of this risk stratification in AML patients aged ≥ 60 years who underwent intensive chemotherapy.
Methods
We retrospectively revised data of 79 patients with new diagnosis of AML since 01/01/2015, followed at AORN Cardarelli Hospital, Naples. The inclusion criteria were age ≥60 years, Eastern Cooperative Oncology Group (ECOG) score ≤2, intensive chemotherapy as frontline approach. Patients were risk stratified according to ELN 2017 recommendations.
Results
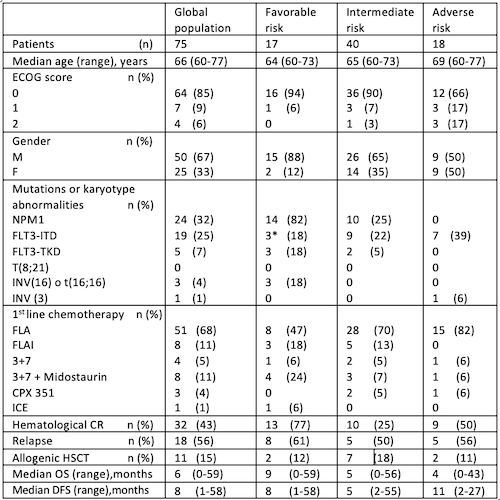
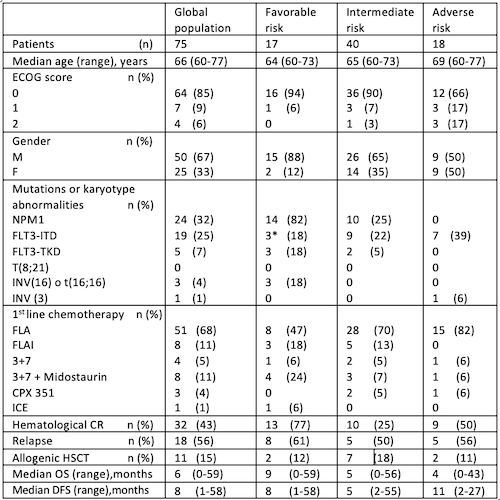
Patients and disease characteristics are summarized in Table1. The median age of the entire population was 66 years (60-77). Mutations in NPM1 and FLT3-ITD were detected in 24/75 (32%) and 19/75 (25%) cases.
Patients were classified, according to ELN 2017 stratification, as follows: 17/75 (23%) favourable, 40/75 (53%) intermediate and 18/75 (24%) adverse risk. A hematologic al complete response (CR) after induction treatment was achieved by 32/75 (43%) patients and was significantly associated with favourable ELN 2017 risk (p=0.03).The median Overall Survival (mOS) of the entire population was 6 months (0-59)(CI:4.82-7.10). The ELN2017 stratified mOS was 9 (0-59) for favourable, 5 (0-56) for intermediate and 4 months (0-43) for adverse risk AML (p=0.1). Particularly, the difference in mOS resulted significant in comparing the favourable to intermediate+adverse risk AML (9 vs 5 months; p=0.038).
No significant differences in terms of mOS were observed between NPM1 mutated vs unmutated (7 vs 6 months; p=0.806) or FLT3-ITD mutated vs unmutated AML (2 vs 6 months; p=0.119), respectively.
In multivariate analysis, the only conditions significantly related to longer OS were the allogenic hematopoietic stem cell transplantation (HSCT)(median OS not reached;HR:15.19;CI:3.34-69.05;p<0.005) and a CR after induction therapy (median OS 11months;HR:2.55;CI:1.30-5.00;p=0.006), while belonging to ELN 2017 favourable risk compared to intermediate+adverse risk AML was not significant (median OS 9 months; HR:0.58;CI:0.25-1.35; p=0.201).
The median Disease-Free Survival (mDFS) of the entire population was 8 months (1-58)(CI:3,92-12,07). No significant differences were found among the ELN2017 groups in mDFS. In multivariate analysis no variables resulted significantly associated with longer DSF.
Conclusion
Our study demonstrated only the ELN2017 favourable risk had a significant benefit in terms of CR rate and mOS but not mDFS in patients aged ≥60 years with AML diagnosis who underwent intensive chemotherapy as frontline approach. The outcome of ELN2017 intermediate and adverse risk AML was very poor, without any difference between the two risk classes. Interestingly, NPM1 or FLT3-ITD mutations added no significant variation in terms of mOS or mDFS, while a significant impact of HSCT still remained.
Our results finally showed how prognostic significance of genetic abnormalities in AML might be influenced by age, and that a new risk stratification integrating performance status, age, presence of targetable mutations by tyrosine kinase inhibitors and transplant eligibility should be considered in setting of elderly patients.
Keyword(s): AML, Chemotherapy, Cytogenetic abnormalities, Elderly
Abstract: PB1392
Type: Publication Only
Session title: Acute myeloid leukemia - Clinical
Background
Acute Myeloid Leukemia (AML) is a bone marrow clonal disorder characterized by the proliferation of myeloid blasts. The European LeukemiaNet (ELN) 2017 risk stratification is a consolidated prognostic system focused on AML genetic features which is able to predict the probability of AML response and relapse following an intensive chemotherapeutic approach.
However, chemosensitivity and risk of disease relapse is age-dependent and limited for patient aged up to 60 years.
Aims
We investigated the predictability of this risk stratification in AML patients aged ≥ 60 years who underwent intensive chemotherapy.
Methods
We retrospectively revised data of 79 patients with new diagnosis of AML since 01/01/2015, followed at AORN Cardarelli Hospital, Naples. The inclusion criteria were age ≥60 years, Eastern Cooperative Oncology Group (ECOG) score ≤2, intensive chemotherapy as frontline approach. Patients were risk stratified according to ELN 2017 recommendations.
Results
Patients and disease characteristics are summarized in Table1. The median age of the entire population was 66 years (60-77). Mutations in NPM1 and FLT3-ITD were detected in 24/75 (32%) and 19/75 (25%) cases.
Patients were classified, according to ELN 2017 stratification, as follows: 17/75 (23%) favourable, 40/75 (53%) intermediate and 18/75 (24%) adverse risk. A hematologic al complete response (CR) after induction treatment was achieved by 32/75 (43%) patients and was significantly associated with favourable ELN 2017 risk (p=0.03).The median Overall Survival (mOS) of the entire population was 6 months (0-59)(CI:4.82-7.10). The ELN2017 stratified mOS was 9 (0-59) for favourable, 5 (0-56) for intermediate and 4 months (0-43) for adverse risk AML (p=0.1). Particularly, the difference in mOS resulted significant in comparing the favourable to intermediate+adverse risk AML (9 vs 5 months; p=0.038).
No significant differences in terms of mOS were observed between NPM1 mutated vs unmutated (7 vs 6 months; p=0.806) or FLT3-ITD mutated vs unmutated AML (2 vs 6 months; p=0.119), respectively.
In multivariate analysis, the only conditions significantly related to longer OS were the allogenic hematopoietic stem cell transplantation (HSCT)(median OS not reached;HR:15.19;CI:3.34-69.05;p<0.005) and a CR after induction therapy (median OS 11months;HR:2.55;CI:1.30-5.00;p=0.006), while belonging to ELN 2017 favourable risk compared to intermediate+adverse risk AML was not significant (median OS 9 months; HR:0.58;CI:0.25-1.35; p=0.201).
The median Disease-Free Survival (mDFS) of the entire population was 8 months (1-58)(CI:3,92-12,07). No significant differences were found among the ELN2017 groups in mDFS. In multivariate analysis no variables resulted significantly associated with longer DSF.
Conclusion
Our study demonstrated only the ELN2017 favourable risk had a significant benefit in terms of CR rate and mOS but not mDFS in patients aged ≥60 years with AML diagnosis who underwent intensive chemotherapy as frontline approach. The outcome of ELN2017 intermediate and adverse risk AML was very poor, without any difference between the two risk classes. Interestingly, NPM1 or FLT3-ITD mutations added no significant variation in terms of mOS or mDFS, while a significant impact of HSCT still remained.
Our results finally showed how prognostic significance of genetic abnormalities in AML might be influenced by age, and that a new risk stratification integrating performance status, age, presence of targetable mutations by tyrosine kinase inhibitors and transplant eligibility should be considered in setting of elderly patients.
Keyword(s): AML, Chemotherapy, Cytogenetic abnormalities, Elderly


