
Contributions
Abstract: PB2525
Type: Publication Only
Background
In this survey we included patients with clinical indications for liver transplant (LT) and concomitant hematological disorders. End-stage liver diseases were alcoholic and viral cirrhoses (A&VC), hepatocellular carcinoma (HCC), Budd-Chiari syndrome (BCS), primary biliary cirrhosis (PBC), primary sclerosing cholangitis (PSC), cirrhosis and cholestatic liver disease (C&CLD), familial amyloid polyneuropathy (FAP), arteriovenous malformations (AVM), and hepatic toxicity (HT). Blood disorders were hemochromatosis, Osler-Weber-Rendu disease (OWRD), hemophilia B, myeloproliferative syndromes (MPS) including chronic myeloid leukemia (CML) submitted to bone marrow transplantation (BMT), polycythemia vera (PV) and essential thrombocythemia (ET), myelodysplastic syndrome (MDS), β-thalassemia minor, sickle cell disease (SCD), immune thrombocytopenic purpura (ITP), and acute myeloid leukemia subtype M2 (AML-M2) treated with BMT in childhood.
Aims
A series of 35 consecutive patients with hematological diseases submitted to LT was retrospectively analyzed (group A). In this set of patients, 35 primary transplants were done with grafts from different sources: cadaveric (32), related healthy living-donor (1), non-related healthy living-donor (1) and FAP carrier donor (1). A total of 5 re-transplants (all from cadaver) were performed. Main goals were to detect differences in transfusion supply comparing 127 patients with A&VC and/or HCC only (group B) with 21 hematological patients with the same liver diagnoses (group C) and their mortality rates. Consumptions and overall survival were also considered in group A.
Methods
A review of electronic clinical records was carried out in patients whose LT were comprised between 1 February 2010 and 31 January 2017 (one or more years following patient’s last LT) in CHLC. Specific archives of the Department of Immunohemotherapy were assessed.
Results
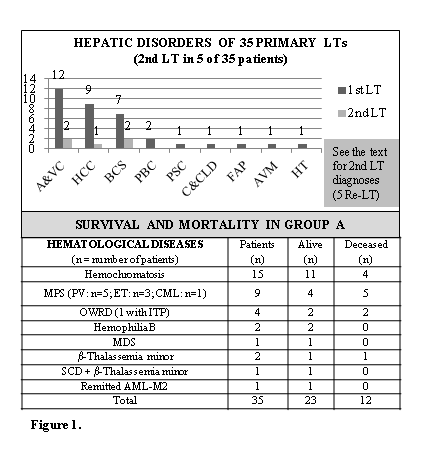
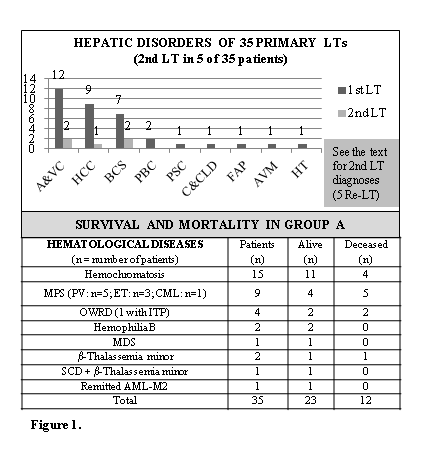
The enrolled hematological patients (group A) were 21 males and 14 females (mean: 49.9; SD: 10.2 years-old). From group A and concerning A&VC and/or HCC, 18 males and 3 females (mean: 54.1; SD: 7.4 years-old) corresponded to group C which were compared to 109 males and 18 females (mean: 55.7; SD: 8.3 years-old) identified as group B during corresponding months of LT. In hematological patients, the distribution of hepatic disorders related to the 1st LT is displayed (figure 1). Diagnoses for the 2nd LT were arterial and venous thrombosis, graft fibrosing cholestatic hepatitis and acute graft failure. A&VC without HCC were clustered in one column and HCC (alone/associated with cirrhoses) in another column. Hematological diagnoses, survival and mortality are presented (figure 1). All-causes mortality rates were 25.2% and 19.0% in groups B and C respectively. Consumption medians in group B were 6 red blood cell units and 20 plasma units versus 3 and 14 units in group C and 4 and 18 units in group A, respectively. More products were also provided for bleeding control.
Conclusion
Overall survival in group A corresponded to 65.7% and mortality rate reached 34.3% which was related to hepatic disorder in the majority of patients. The leading causes of death were hemorrhagic shock (all groups) followed by severe infection (group B); one case of CML relapse and another of sepsis occurred in group A. The hematological patients showed a lower blood transfusion support. MPS were associated with BCS in 7 patients. Severe diseases can be treated by a multidisciplinary management with net clinical benefits. Creating new synergies could improve outcomes of hematological patients needing LT.
Session topic: 32. Transfusion medicine
Keyword(s): Blood transfusion, Liver disease, Liver transplant, Survival
Abstract: PB2525
Type: Publication Only
Background
In this survey we included patients with clinical indications for liver transplant (LT) and concomitant hematological disorders. End-stage liver diseases were alcoholic and viral cirrhoses (A&VC), hepatocellular carcinoma (HCC), Budd-Chiari syndrome (BCS), primary biliary cirrhosis (PBC), primary sclerosing cholangitis (PSC), cirrhosis and cholestatic liver disease (C&CLD), familial amyloid polyneuropathy (FAP), arteriovenous malformations (AVM), and hepatic toxicity (HT). Blood disorders were hemochromatosis, Osler-Weber-Rendu disease (OWRD), hemophilia B, myeloproliferative syndromes (MPS) including chronic myeloid leukemia (CML) submitted to bone marrow transplantation (BMT), polycythemia vera (PV) and essential thrombocythemia (ET), myelodysplastic syndrome (MDS), β-thalassemia minor, sickle cell disease (SCD), immune thrombocytopenic purpura (ITP), and acute myeloid leukemia subtype M2 (AML-M2) treated with BMT in childhood.
Aims
A series of 35 consecutive patients with hematological diseases submitted to LT was retrospectively analyzed (group A). In this set of patients, 35 primary transplants were done with grafts from different sources: cadaveric (32), related healthy living-donor (1), non-related healthy living-donor (1) and FAP carrier donor (1). A total of 5 re-transplants (all from cadaver) were performed. Main goals were to detect differences in transfusion supply comparing 127 patients with A&VC and/or HCC only (group B) with 21 hematological patients with the same liver diagnoses (group C) and their mortality rates. Consumptions and overall survival were also considered in group A.
Methods
A review of electronic clinical records was carried out in patients whose LT were comprised between 1 February 2010 and 31 January 2017 (one or more years following patient’s last LT) in CHLC. Specific archives of the Department of Immunohemotherapy were assessed.
Results
The enrolled hematological patients (group A) were 21 males and 14 females (mean: 49.9; SD: 10.2 years-old). From group A and concerning A&VC and/or HCC, 18 males and 3 females (mean: 54.1; SD: 7.4 years-old) corresponded to group C which were compared to 109 males and 18 females (mean: 55.7; SD: 8.3 years-old) identified as group B during corresponding months of LT. In hematological patients, the distribution of hepatic disorders related to the 1st LT is displayed (figure 1). Diagnoses for the 2nd LT were arterial and venous thrombosis, graft fibrosing cholestatic hepatitis and acute graft failure. A&VC without HCC were clustered in one column and HCC (alone/associated with cirrhoses) in another column. Hematological diagnoses, survival and mortality are presented (figure 1). All-causes mortality rates were 25.2% and 19.0% in groups B and C respectively. Consumption medians in group B were 6 red blood cell units and 20 plasma units versus 3 and 14 units in group C and 4 and 18 units in group A, respectively. More products were also provided for bleeding control.
Conclusion
Overall survival in group A corresponded to 65.7% and mortality rate reached 34.3% which was related to hepatic disorder in the majority of patients. The leading causes of death were hemorrhagic shock (all groups) followed by severe infection (group B); one case of CML relapse and another of sepsis occurred in group A. The hematological patients showed a lower blood transfusion support. MPS were associated with BCS in 7 patients. Severe diseases can be treated by a multidisciplinary management with net clinical benefits. Creating new synergies could improve outcomes of hematological patients needing LT.
Session topic: 32. Transfusion medicine
Keyword(s): Blood transfusion, Liver disease, Liver transplant, Survival


