
Contributions
Abstract: PB2535
Type: Publication Only
Background
Blood transfusion is an essential treatment, sometimes the only valid one, but it always involves certain risks. Physicians should weigh in the benefits and hazards of this treatment and follow the recommendations. Most studies demonstrate that in recent years, red cell transfusion has decreased, meanwhile platelet transfusion remains practically the same. This is because of the application of smarter blood transfusion protocols.
Aims
Make a retrospective study of red cell and platelet transfusion in our hospital. We analyzed hemoglobin levels and number of platelets before and after transfusion; we also analyzed the type of surgery, medical disorder and mortality, among other variables.
Methods
We collected data of red cell and platelet transfusion at Vigo hospital, from January to June 2016. We did a descriptive analysis, presenting qualitative variables as absolute frequency and percentage, and quantitative variables as mean and standard deviation. We used Chi square test to compare qualitative variables between types of surgery and also between the various medical disorders. We used one factor ANOVA to compare quantitative variables. Data were analyzed with IBM SPSS statistics 19.0. The accepted level of statistical significance was 0.05.
Results
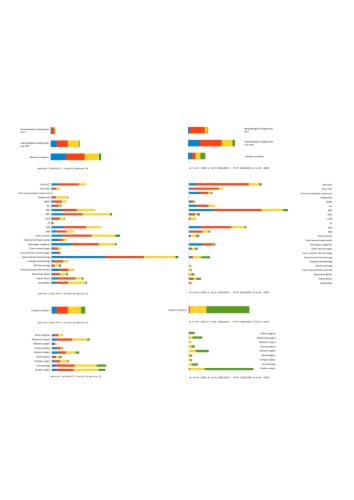
We transfused 7787 blood products to 1575 patients; 6175 packed red cells and 1612 platelets. 51.4% of patients were male. Mean age was 69+/-19,6. Most of red cell transfusions were to patients with medical disorders, and among them, to patients with hematological ones. In patients with non hematological medical disorders, most of transfusions were to those with GI bleeding, followed by solid organ cancer. On the other hand, most platelet transfusions were to patients with solid organ malignancies, follow by patients with non hematological anemia (Graphics 1). Patients with hematological disorders which received the most red cell transfusions were, in order: MDS, NHL, acute myeloid leukemia and allogenic stem cell transplantation. Regarding platelet transfusions, the order is the following: acute myeloid leukemia, allogenic stem transplantation, NHL and autologous stem cell transplantation. Among surgical patients, the ones which received most of red cell transfusions were trauma patients, follow by cardiac and abdominal surgeries; platelet transfusions were received mostly by patients undergoing cardiac surgery, follow by vascular surgery. Other variables, such as anticoagulation or infection, didn't have clinical significance over transfusion. Most deaths occurred in the group of patients with medical conditions (71,2%), and among those, the ones with solid organ malignancies, follow by non hematological anemias and GI bleeding. Regarding these results we could identified inadequate transfusion behaviors.
Conclusion
In our hospital, we concluded that patients who received the most transfusions were those with medical conditions, and among them, the ones with hematological disorders. These results are similar to those published in other studies. Nevertheless, platelet transfusions were received in large numbers by patients with a number above 50.000, which is not what guidelines recommend. On the other hand, red cell transfusion, in our hospital, is closer to the recommendations, even if we have a liberal transfusion policy. These findings led us to apply some corrective actions in our hospital.
Session topic: 32. Transfusion medicine
Abstract: PB2535
Type: Publication Only
Background
Blood transfusion is an essential treatment, sometimes the only valid one, but it always involves certain risks. Physicians should weigh in the benefits and hazards of this treatment and follow the recommendations. Most studies demonstrate that in recent years, red cell transfusion has decreased, meanwhile platelet transfusion remains practically the same. This is because of the application of smarter blood transfusion protocols.
Aims
Make a retrospective study of red cell and platelet transfusion in our hospital. We analyzed hemoglobin levels and number of platelets before and after transfusion; we also analyzed the type of surgery, medical disorder and mortality, among other variables.
Methods
We collected data of red cell and platelet transfusion at Vigo hospital, from January to June 2016. We did a descriptive analysis, presenting qualitative variables as absolute frequency and percentage, and quantitative variables as mean and standard deviation. We used Chi square test to compare qualitative variables between types of surgery and also between the various medical disorders. We used one factor ANOVA to compare quantitative variables. Data were analyzed with IBM SPSS statistics 19.0. The accepted level of statistical significance was 0.05.
Results
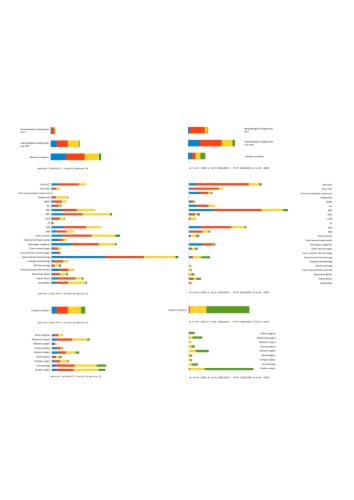
We transfused 7787 blood products to 1575 patients; 6175 packed red cells and 1612 platelets. 51.4% of patients were male. Mean age was 69+/-19,6. Most of red cell transfusions were to patients with medical disorders, and among them, to patients with hematological ones. In patients with non hematological medical disorders, most of transfusions were to those with GI bleeding, followed by solid organ cancer. On the other hand, most platelet transfusions were to patients with solid organ malignancies, follow by patients with non hematological anemia (Graphics 1). Patients with hematological disorders which received the most red cell transfusions were, in order: MDS, NHL, acute myeloid leukemia and allogenic stem cell transplantation. Regarding platelet transfusions, the order is the following: acute myeloid leukemia, allogenic stem transplantation, NHL and autologous stem cell transplantation. Among surgical patients, the ones which received most of red cell transfusions were trauma patients, follow by cardiac and abdominal surgeries; platelet transfusions were received mostly by patients undergoing cardiac surgery, follow by vascular surgery. Other variables, such as anticoagulation or infection, didn't have clinical significance over transfusion. Most deaths occurred in the group of patients with medical conditions (71,2%), and among those, the ones with solid organ malignancies, follow by non hematological anemias and GI bleeding. Regarding these results we could identified inadequate transfusion behaviors.
Conclusion
In our hospital, we concluded that patients who received the most transfusions were those with medical conditions, and among them, the ones with hematological disorders. These results are similar to those published in other studies. Nevertheless, platelet transfusions were received in large numbers by patients with a number above 50.000, which is not what guidelines recommend. On the other hand, red cell transfusion, in our hospital, is closer to the recommendations, even if we have a liberal transfusion policy. These findings led us to apply some corrective actions in our hospital.
Session topic: 32. Transfusion medicine


