
Contributions
Abstract: PB2537
Type: Publication Only
Background
The benefit of Plasma Exchange (PE) in acute kidney injury secondary to vasculitis has been demonstrated both in the acute phase of these diseases, but also has been proved to decrease the dialysis-dependent rate at the first year.
Aims
The aim of this article is to evaluate the safe of PE in renal vasculitis, and secondarily the response (dialysis independence) at 30 days.
Methods
Unicentre descriptive and longitudinal study, with a prospective database of all patients with acute renal failure secondary to vasculitis treated with PE. severity of renal injury was classified according to AKIN (Acute Kidney Injury Network) scale and RIFLE (Risk, Injury, Failure, Loss y End Stage Kidney Disease risk, Injury) criteria.
Results
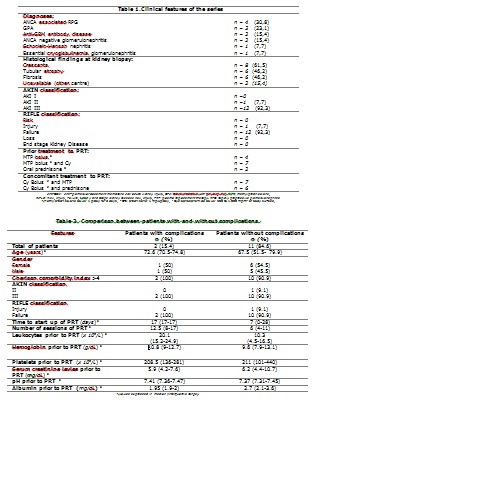
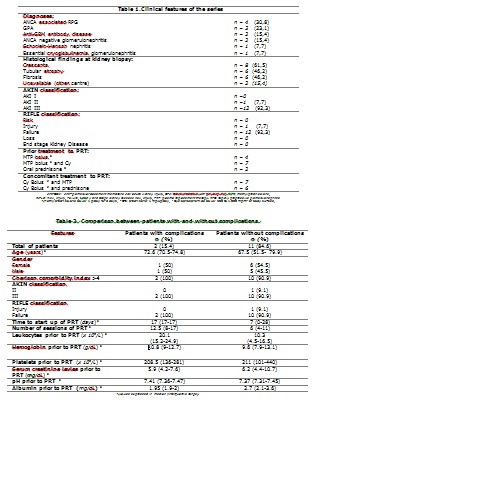
We analysed 13 cases, 7 women. The median age was 67.7 years, 30-day response rate were 38.5% and 92.3% had a high Charlson comorbidity index (>4). All patients needed dyalisis but only in 4 were performed before the onset of PE. Other clinical characteristics are exposed at table 1. Serum creatinine levels below 5.8 mg/dL were related with great responses (p=0.032). There were observed decreases of serum creatinine levels (p=0.005), glomerular filtrate (p=0.003) and random urine sample proteinuria (p=0.045). The devices used for PE were continous-flow cell separators. The standard replacement solution is 5% human albumin. To avoid hypocalcemia symptoms, intravenous calcium gluconate is administered as prophylaxis at the beginning of each session and is repeated if symptoms appear. In accordance with the local protocol to prevent dilutional coagulopathy, all patients receive intravenous vitamin K at the end of the procedure. A median of 6 (4-17) sessions were performed per patient and were initiated 10 (0-28) days after diagnosis. Out of the 96 sessions carried out, one (1.04%) presented a low access pressure and 4 (4.1%) clinical complications (itching in 3 and fever in 1), corresponding to two patients (table 2). None of them were serious and only one had to be suspended due to fever. Patients who experience more complications (clinical and technical) had a high number of leukocytes prior to PRT (p=0.04) and had undergone a higher number of sessions (p=0.010) as showed in table 2.
Conclusion
Global frequency of complications in our series was lower than published in the literature, it leads us to conclude that PRT is a safe therapeutic strategy in our centre and encourages us to postulate that our prophylactic measures. The finding of increased initial white blood cell count in patients with complications, might be investigated in studies with higher casuistry.
Session topic: 32. Transfusion medicine
Keyword(s): Plasma, Renal failure
Abstract: PB2537
Type: Publication Only
Background
The benefit of Plasma Exchange (PE) in acute kidney injury secondary to vasculitis has been demonstrated both in the acute phase of these diseases, but also has been proved to decrease the dialysis-dependent rate at the first year.
Aims
The aim of this article is to evaluate the safe of PE in renal vasculitis, and secondarily the response (dialysis independence) at 30 days.
Methods
Unicentre descriptive and longitudinal study, with a prospective database of all patients with acute renal failure secondary to vasculitis treated with PE. severity of renal injury was classified according to AKIN (Acute Kidney Injury Network) scale and RIFLE (Risk, Injury, Failure, Loss y End Stage Kidney Disease risk, Injury) criteria.
Results
We analysed 13 cases, 7 women. The median age was 67.7 years, 30-day response rate were 38.5% and 92.3% had a high Charlson comorbidity index (>4). All patients needed dyalisis but only in 4 were performed before the onset of PE. Other clinical characteristics are exposed at table 1. Serum creatinine levels below 5.8 mg/dL were related with great responses (p=0.032). There were observed decreases of serum creatinine levels (p=0.005), glomerular filtrate (p=0.003) and random urine sample proteinuria (p=0.045). The devices used for PE were continous-flow cell separators. The standard replacement solution is 5% human albumin. To avoid hypocalcemia symptoms, intravenous calcium gluconate is administered as prophylaxis at the beginning of each session and is repeated if symptoms appear. In accordance with the local protocol to prevent dilutional coagulopathy, all patients receive intravenous vitamin K at the end of the procedure. A median of 6 (4-17) sessions were performed per patient and were initiated 10 (0-28) days after diagnosis. Out of the 96 sessions carried out, one (1.04%) presented a low access pressure and 4 (4.1%) clinical complications (itching in 3 and fever in 1), corresponding to two patients (table 2). None of them were serious and only one had to be suspended due to fever. Patients who experience more complications (clinical and technical) had a high number of leukocytes prior to PRT (p=0.04) and had undergone a higher number of sessions (p=0.010) as showed in table 2.
Conclusion
Global frequency of complications in our series was lower than published in the literature, it leads us to conclude that PRT is a safe therapeutic strategy in our centre and encourages us to postulate that our prophylactic measures. The finding of increased initial white blood cell count in patients with complications, might be investigated in studies with higher casuistry.
Session topic: 32. Transfusion medicine
Keyword(s): Plasma, Renal failure


