
Contributions
Abstract: PB2438
Type: Publication Only
Background
The growing threat of colonization by multidrug resistant organisms (MDRO) presents a particular challenge to haemato-oncology patients receiving chemotherapy or undergoing a haematopoietic stem cell transplantation (HSCT) as they are heavily reliant on antimicrobial agents to prevent and treat overwhelming infection. MDRO include carbapenem producing Enterobacteriaceae (CPE) and vancomycin-resistant Enterococci (VRE) and both can colonise the bowel. Haemato-oncology patients often develop prolonged neutropenia and gastrointestinal mucositis which creates the perfect means for translocation of these MDRO and can lead to systemic infection. There are few studies examining the impact of multi-faceted infection prevention and control bundles on MDRO colonisation and infection in haemato-oncology patients.
Aims
To assess the impact of the introduction of a bundle of infection prevention and control measures on CPE and VRE colonisation and infection rates in haemato-oncology patients.
Methods
Data on MDRO colonisation and infection of consecutive patients receiving treatment in our haematology ward between April 2012 and December 2017 was collected. An intervention consisting of 15 infection prevention and control measures, such as patient and staff cohorting and the use of a vapourised hydrogen peroxide system was introduced in November 2014. Patients were divided into pre and post intervention cohorts and the incidence of new CPE and VRE colonisation compared. Secondary outcomes include the incidence of MDRO infection and hand hygiene compliance. Statistical analysis was carried out using SPSS version 22 and Mann Whitney U test was used to compare colonisation and infection incidence between pre and post intervention periods.
Results
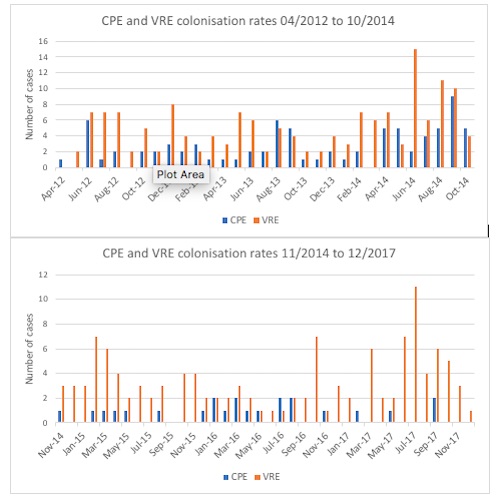
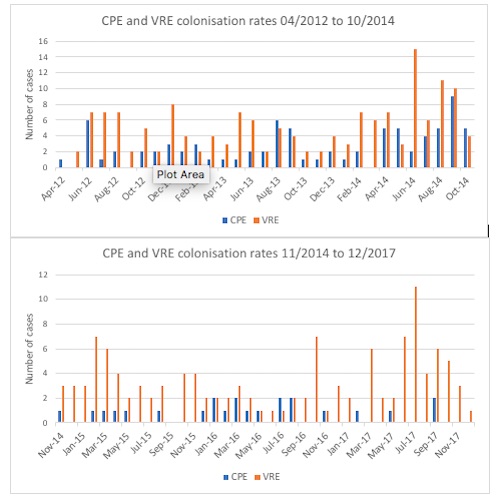
During the 69 month period of the study, there were 41,594 patient days; 20,768 in the pre-intervention period and 20,826 in the post intervention period. Monthly acquisition of CPE and VRE colonisation for the two study periods is shown in figure 1. The total number of CPE colonisation acquisitions over the whole study period was 105; 82 in the pre-intervention period and 23 in the post intervention period. The incidence density of CPE colonisation acquisition in the pre-intervention period was 3.95 cases per 1000 patient days compared to 1.1 cases per 1000 patient days in the post intervention period (p=0.0001). The total number of VRE colonisation acquisitions over the study period was 279; 157 in the pre-intervention period and 122 in the post-intervention period. The incidence density of VRE colonisation acquisition in the pre-intervention period was 7.6 cases per 1000 patient days compared to 5.9 cases per 1000 patient days in the post intervention period (p=0.12).
Conclusion
The implementation of a multi-faceted bundle of infection prevention and control measures led to a significant reduction in new colonisation with CPE in our haemato-oncology cohort. In contrast, the incidence density of new VRE colonisation showed no statistically significant decrease. This may reflect differences between CPE and VRE in mode of transmission and susceptibility to particular infection control measures. Since the main source of MDRO infection in this cohort is thought to be mucositis related, we expect the significant reduction in CPE colonisation to be matched by a similar reduction in CPE infection. This emphasises the importance of rigorous infection prevention and control measures in protecting our patients in the age of the superbug.
Session topic: 23. Stem cell transplantation - Clinical
Keyword(s): Infection, Multidrug resistance, Stem cell transplant
Abstract: PB2438
Type: Publication Only
Background
The growing threat of colonization by multidrug resistant organisms (MDRO) presents a particular challenge to haemato-oncology patients receiving chemotherapy or undergoing a haematopoietic stem cell transplantation (HSCT) as they are heavily reliant on antimicrobial agents to prevent and treat overwhelming infection. MDRO include carbapenem producing Enterobacteriaceae (CPE) and vancomycin-resistant Enterococci (VRE) and both can colonise the bowel. Haemato-oncology patients often develop prolonged neutropenia and gastrointestinal mucositis which creates the perfect means for translocation of these MDRO and can lead to systemic infection. There are few studies examining the impact of multi-faceted infection prevention and control bundles on MDRO colonisation and infection in haemato-oncology patients.
Aims
To assess the impact of the introduction of a bundle of infection prevention and control measures on CPE and VRE colonisation and infection rates in haemato-oncology patients.
Methods
Data on MDRO colonisation and infection of consecutive patients receiving treatment in our haematology ward between April 2012 and December 2017 was collected. An intervention consisting of 15 infection prevention and control measures, such as patient and staff cohorting and the use of a vapourised hydrogen peroxide system was introduced in November 2014. Patients were divided into pre and post intervention cohorts and the incidence of new CPE and VRE colonisation compared. Secondary outcomes include the incidence of MDRO infection and hand hygiene compliance. Statistical analysis was carried out using SPSS version 22 and Mann Whitney U test was used to compare colonisation and infection incidence between pre and post intervention periods.
Results
During the 69 month period of the study, there were 41,594 patient days; 20,768 in the pre-intervention period and 20,826 in the post intervention period. Monthly acquisition of CPE and VRE colonisation for the two study periods is shown in figure 1. The total number of CPE colonisation acquisitions over the whole study period was 105; 82 in the pre-intervention period and 23 in the post intervention period. The incidence density of CPE colonisation acquisition in the pre-intervention period was 3.95 cases per 1000 patient days compared to 1.1 cases per 1000 patient days in the post intervention period (p=0.0001). The total number of VRE colonisation acquisitions over the study period was 279; 157 in the pre-intervention period and 122 in the post-intervention period. The incidence density of VRE colonisation acquisition in the pre-intervention period was 7.6 cases per 1000 patient days compared to 5.9 cases per 1000 patient days in the post intervention period (p=0.12).
Conclusion
The implementation of a multi-faceted bundle of infection prevention and control measures led to a significant reduction in new colonisation with CPE in our haemato-oncology cohort. In contrast, the incidence density of new VRE colonisation showed no statistically significant decrease. This may reflect differences between CPE and VRE in mode of transmission and susceptibility to particular infection control measures. Since the main source of MDRO infection in this cohort is thought to be mucositis related, we expect the significant reduction in CPE colonisation to be matched by a similar reduction in CPE infection. This emphasises the importance of rigorous infection prevention and control measures in protecting our patients in the age of the superbug.
Session topic: 23. Stem cell transplantation - Clinical
Keyword(s): Infection, Multidrug resistance, Stem cell transplant


