
Contributions
Abstract: PB2431
Type: Publication Only
Background
Treatments for multiple myeloma (MM) with induction chemotherapy followed by autologous stem cell transplantation (ASCT) and maintenance therapy have been recommended as the standard approach. Long term follow-up after transplantation and factors associated with progression-free survival (PFS) and overall survival (OS) are not yet elucidated.
Aims
To investigate long term transplantation outcome including OS, PFS and related prognostic factors in patients with newly diagnosed MM who underwent ASCT in a referral university hospital in Thailand.
Methods
A cohort of patients older than 18 years with first diagnosed MM treated with ASCT from 2000 to 2015 were reviewed. We used IMWG criteria to classify the depth of response. All patients received induction regimen(s) comprising 2 or 3 drugs followed by high-dose melphalan before undergoing ASCT. Factors affecting survival were explored using Cox proportional hazard models.
Results
One hundred and twenty-two patients were included. The median follow-up time was 39 (2-115) months. The median age of the cohort was 56 (31-68) years with 45.1% of male. IgG Kappa was the most common type of paraprotein identified. Majority of patients were in ISS stage III (34.4%) followed by stage II and I at 21.3 and 14.8 %, respectively. Approximately half of patients (48%) received only 1-drug regimen before ASCT. Most patients (92%) received novel agent(s) for which bortezomib was the most commonly used drug (87%), either as a single agent or in combination. Thalidomide or lenalidomide was used 30% and 18%, respectively. Prior to ASCT; 63.1%, 5.7%, 26.2% and 4.9% of subjects achieved sCR, CR, VGPR and PR, respectively. After ASCT; 68.9%, 4.9%, 23.7% and 3.3% of subjects achieved sCR, CR, VGPR and PR, respectively. There was no transplantation-related mortality. ASCT improved disease response in 22/45(49%) patients who achieved less than sCR before ASCT. After ASCT, 24.6% received consolidation and 52.5% received maintenance therapy.
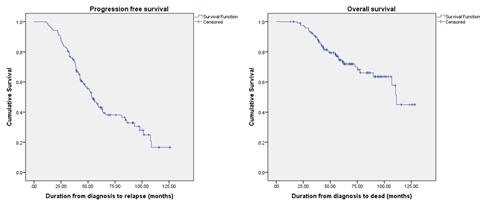
Median OS was 111.3 months while 3-yr OS, 5-yr OS and 10-yr OS were 91%, 74%, and 45% respectively. Median PFS was 53.4 months while 3-yr PFS, 5-yr PFS, and 10-yr PFS were 75%, 43% and 16% respectively. Factors affecting PFS included presence of plasma cells ≥5% in BMA after induction chemotherapy (HR 3.53, 95% CI 1.25-9.93, p = 0.017), or after ASCT (HR 4.29, 95% CI 1.23-14.99, p = 0.022), achieving less than CR after ASCT (HR 2.32, 95% CI 1.35-3.98, p = 0.002), and receiving maintenance therapy (HR 0.35, 95% CI 0.21-0.59, p < 0.001). While male (HR 2.10, 95% CI 1.01-4.37, p = 0.047) and achieving less than VGPR after ASCT (HR 5.72, 95% CI 1.03-31.67, p = 0.046) were affected patients’ OS.
Subgroup analysis showed that maintenance therapy had significant benefit for both OS and PFS only in the patients who achieved VGPR after ASCT (OS_HR 0.115, 95% CI 0.03-0.43, p = 0.001, PFS_HR 0.12, 95% CI 0.05-0.30, p < 0.001). Maintenance with lenalidomide or thalidomide didn’t alter PFS (HR 0.71, 95% CI 0.35-2.06, p = 0.844). Abnormal SFLC had significantly impacted on PFS (HR 2.15, 95% CI 1.24-3.74, p = 0.006).
Conclusion
We reported almost 10-year overall survival in newly diagnosed multiple myeloma treated with upfront autologous stem cell transplantation. Depth of response, either pre or post stem cell transplantation, determines patients’ survival. Moreover, our data revealed that maintenance therapy post transplantation improved clinical outcome, particularly among patients who achieved less than complete response after stem cell transplantation.
Session topic: 23. Stem cell transplantation - Clinical
Keyword(s): Autologous hematopoietic stem cell transplantation, Multiple Myeloma, Prognostic factor, Survival
Abstract: PB2431
Type: Publication Only
Background
Treatments for multiple myeloma (MM) with induction chemotherapy followed by autologous stem cell transplantation (ASCT) and maintenance therapy have been recommended as the standard approach. Long term follow-up after transplantation and factors associated with progression-free survival (PFS) and overall survival (OS) are not yet elucidated.
Aims
To investigate long term transplantation outcome including OS, PFS and related prognostic factors in patients with newly diagnosed MM who underwent ASCT in a referral university hospital in Thailand.
Methods
A cohort of patients older than 18 years with first diagnosed MM treated with ASCT from 2000 to 2015 were reviewed. We used IMWG criteria to classify the depth of response. All patients received induction regimen(s) comprising 2 or 3 drugs followed by high-dose melphalan before undergoing ASCT. Factors affecting survival were explored using Cox proportional hazard models.
Results
One hundred and twenty-two patients were included. The median follow-up time was 39 (2-115) months. The median age of the cohort was 56 (31-68) years with 45.1% of male. IgG Kappa was the most common type of paraprotein identified. Majority of patients were in ISS stage III (34.4%) followed by stage II and I at 21.3 and 14.8 %, respectively. Approximately half of patients (48%) received only 1-drug regimen before ASCT. Most patients (92%) received novel agent(s) for which bortezomib was the most commonly used drug (87%), either as a single agent or in combination. Thalidomide or lenalidomide was used 30% and 18%, respectively. Prior to ASCT; 63.1%, 5.7%, 26.2% and 4.9% of subjects achieved sCR, CR, VGPR and PR, respectively. After ASCT; 68.9%, 4.9%, 23.7% and 3.3% of subjects achieved sCR, CR, VGPR and PR, respectively. There was no transplantation-related mortality. ASCT improved disease response in 22/45(49%) patients who achieved less than sCR before ASCT. After ASCT, 24.6% received consolidation and 52.5% received maintenance therapy.
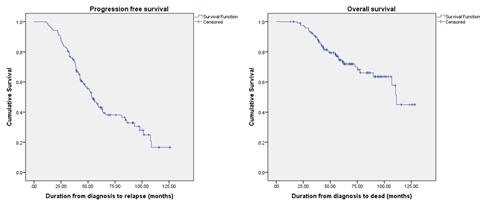
Median OS was 111.3 months while 3-yr OS, 5-yr OS and 10-yr OS were 91%, 74%, and 45% respectively. Median PFS was 53.4 months while 3-yr PFS, 5-yr PFS, and 10-yr PFS were 75%, 43% and 16% respectively. Factors affecting PFS included presence of plasma cells ≥5% in BMA after induction chemotherapy (HR 3.53, 95% CI 1.25-9.93, p = 0.017), or after ASCT (HR 4.29, 95% CI 1.23-14.99, p = 0.022), achieving less than CR after ASCT (HR 2.32, 95% CI 1.35-3.98, p = 0.002), and receiving maintenance therapy (HR 0.35, 95% CI 0.21-0.59, p < 0.001). While male (HR 2.10, 95% CI 1.01-4.37, p = 0.047) and achieving less than VGPR after ASCT (HR 5.72, 95% CI 1.03-31.67, p = 0.046) were affected patients’ OS.
Subgroup analysis showed that maintenance therapy had significant benefit for both OS and PFS only in the patients who achieved VGPR after ASCT (OS_HR 0.115, 95% CI 0.03-0.43, p = 0.001, PFS_HR 0.12, 95% CI 0.05-0.30, p < 0.001). Maintenance with lenalidomide or thalidomide didn’t alter PFS (HR 0.71, 95% CI 0.35-2.06, p = 0.844). Abnormal SFLC had significantly impacted on PFS (HR 2.15, 95% CI 1.24-3.74, p = 0.006).
Conclusion
We reported almost 10-year overall survival in newly diagnosed multiple myeloma treated with upfront autologous stem cell transplantation. Depth of response, either pre or post stem cell transplantation, determines patients’ survival. Moreover, our data revealed that maintenance therapy post transplantation improved clinical outcome, particularly among patients who achieved less than complete response after stem cell transplantation.
Session topic: 23. Stem cell transplantation - Clinical
Keyword(s): Autologous hematopoietic stem cell transplantation, Multiple Myeloma, Prognostic factor, Survival


