
Contributions
Abstract: PB2479
Type: Publication Only
Background
Infections are a major cause of morbidity and mortality in patients with Multiple Myeloma (MM). MM related immunodeficiency involves B-cell dysfunction as well as T-cell, dendritic cell, and NK-cell abnormalities. In addition to the immunodeficiency related to myeloma, the type of anti-myeloma therapy used plays a role in the development of infections.
Aims
To compare transplant outcome in terms of risk of infection between MM patients treated with 2 different frontline therapies.
Methods
Out of 87 MM patients from Hospital Son Llàtzer who underwent ASCT from March 2003 to February 2017, we performed a retrospective observational study involving 35 of them.
Exclusion criteria: patients with Plasma cell leukemia, concomitant diagnosis of Amyloidosis AL and those who received Busulfan-Melfalan as conditioning regimen.
Patients were separated into two groups depending on its frontline therapy (arm A: VBCMP/VBAD vs. arm B: novel agent combinations). Molecular cytogenetic alterations were not included because data for these were not available in all patients. Hematologic recovery was defined as an absolute neutrophil count ≥500/mm3 and platelets ≥20,000/mm3. We analyzed all infections occurred within the first year post-ASCT. In all patients the intensive regimen consisted of Melphalan 200 mg/m2.
Data were collected from electronic medical records. Quantitative variables were expressed as median and interquartile range, and the qualitative variables as percentages (p<0.05 was considered statistically significant). Differences between groups were analyzed with the Mann-Whitney U test and Chi-square.
Results
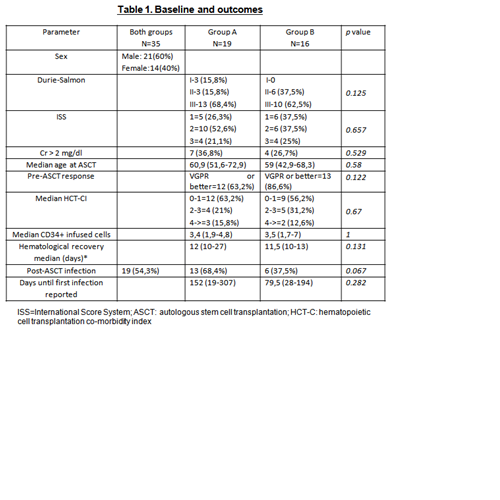
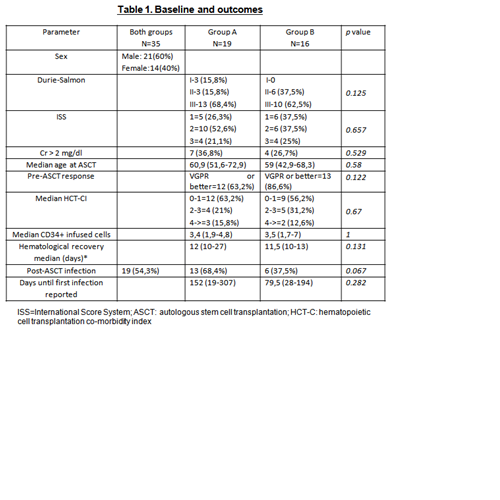
Out of 35 patients analyzed, 19 received poly-chemotherapy as frontline treatment, and 16 patients received combinations of novel agents. No differences were observed between groups in regard to age at the time of transplantation (60.9 years old for group A vs 59 years old for group B) and HCT-CI. In regards to response before ASCT, the rate of very good partial response or better was slightly higher for group B (86.6% vs 63.2%), p=0.122. Median CD34+ infused cells was also similar between groups A and B (3.4.106/kg vs 3.5. 106/kg, respectively. There was no significant difference in hematological recovery (12 vs 11.5 days) or development of mucositis (94.7% vs 100%).
Of 35 patients, 19 (54.3%) developed at least one infectious complication. Although not statistically significant, the frequency of infections was higher in group A (68.4%) than in group B (37.5%), p=0.067. Median time to first infectious episode was 152 days in group A and 79.5 days in group B, p=0.282. Respiratory infections were the most common infections in both groups (33% vs 45.5%), p=0.236. Of note, 3 patients (16.7%) in group A required hospitalization during the first infectious episode vs none in group B, p=0.153.
Conclusion
Infection is a significant cause of morbidity and death in patients with MM.
In this analysis, out of 35 patients, 19 (54.3%) developed at least one infectious complication during the first year after ASCT. Although not statistically significant, the frequency of infections and hospitalization was higher in the group that received poly-chemotherapy, suggesting that poly-chemotherapy might induce more immunosuppression. These results are limited because of the small number of patients included.
Session topic: 23. Stem cell transplantation - Clinical
Keyword(s): Infection, Multiple Myeloma, Stem cell transplant
Abstract: PB2479
Type: Publication Only
Background
Infections are a major cause of morbidity and mortality in patients with Multiple Myeloma (MM). MM related immunodeficiency involves B-cell dysfunction as well as T-cell, dendritic cell, and NK-cell abnormalities. In addition to the immunodeficiency related to myeloma, the type of anti-myeloma therapy used plays a role in the development of infections.
Aims
To compare transplant outcome in terms of risk of infection between MM patients treated with 2 different frontline therapies.
Methods
Out of 87 MM patients from Hospital Son Llàtzer who underwent ASCT from March 2003 to February 2017, we performed a retrospective observational study involving 35 of them.
Exclusion criteria: patients with Plasma cell leukemia, concomitant diagnosis of Amyloidosis AL and those who received Busulfan-Melfalan as conditioning regimen.
Patients were separated into two groups depending on its frontline therapy (arm A: VBCMP/VBAD vs. arm B: novel agent combinations). Molecular cytogenetic alterations were not included because data for these were not available in all patients. Hematologic recovery was defined as an absolute neutrophil count ≥500/mm3 and platelets ≥20,000/mm3. We analyzed all infections occurred within the first year post-ASCT. In all patients the intensive regimen consisted of Melphalan 200 mg/m2.
Data were collected from electronic medical records. Quantitative variables were expressed as median and interquartile range, and the qualitative variables as percentages (p<0.05 was considered statistically significant). Differences between groups were analyzed with the Mann-Whitney U test and Chi-square.
Results
Out of 35 patients analyzed, 19 received poly-chemotherapy as frontline treatment, and 16 patients received combinations of novel agents. No differences were observed between groups in regard to age at the time of transplantation (60.9 years old for group A vs 59 years old for group B) and HCT-CI. In regards to response before ASCT, the rate of very good partial response or better was slightly higher for group B (86.6% vs 63.2%), p=0.122. Median CD34+ infused cells was also similar between groups A and B (3.4.106/kg vs 3.5. 106/kg, respectively. There was no significant difference in hematological recovery (12 vs 11.5 days) or development of mucositis (94.7% vs 100%).
Of 35 patients, 19 (54.3%) developed at least one infectious complication. Although not statistically significant, the frequency of infections was higher in group A (68.4%) than in group B (37.5%), p=0.067. Median time to first infectious episode was 152 days in group A and 79.5 days in group B, p=0.282. Respiratory infections were the most common infections in both groups (33% vs 45.5%), p=0.236. Of note, 3 patients (16.7%) in group A required hospitalization during the first infectious episode vs none in group B, p=0.153.
Conclusion
Infection is a significant cause of morbidity and death in patients with MM.
In this analysis, out of 35 patients, 19 (54.3%) developed at least one infectious complication during the first year after ASCT. Although not statistically significant, the frequency of infections and hospitalization was higher in the group that received poly-chemotherapy, suggesting that poly-chemotherapy might induce more immunosuppression. These results are limited because of the small number of patients included.
Session topic: 23. Stem cell transplantation - Clinical
Keyword(s): Infection, Multiple Myeloma, Stem cell transplant


