
Contributions
Abstract: PB1773
Type: Publication Only
Background
Primary Pancreatic Lymphoma (PPL) is a very rare disease, representing only 0.1% of lymphomas and 0.2% of pancreatic tumors. According to the WHO classification the diagnostic criteria for PPL are: i) the bulk of the disease has to localize in the pancreas; ii) although adjacent and distant spread may be exist the primary clinical presentation has to involve the pancreatic gland. PPL presentation is variable and may overlap the onset of other neoplastic or inflammatory pancreatic diseases, often resulting in diagnostic difficulties. Histopathological examination usually reveals a diffuse large B cell lymphoma (DLBCL), nonetheless other types of lymphomas have been reported including the indolent ones. Diagnosis can be obtained through a percutaneous/endoscopic ultrasound-guided biopsy or surgery. An accurate histological characterization is essential because, unlike epithelial tumors, PPL does not benefit from surgery.
Aims
to evaluate retrospectively clinical, laboratory and histological characteristics, diagnosis, treatment, and outcome of a series of PPL patients diagnosed in 2 hematology units.
Methods
patients diagnosed with PPL between 2008 and 2017 were retrieved from the medical record databases of the Verona and Vicenza Hematology Units. Inclusion criteria were the availability of information related to clinical onset, histopathological diagnosis, laboratory tests, radiology imaging, treatment and follow-up. Patients with secondary pancreatic involvement of lymphoma were excluded. All cases herein presented were revised to ensure that they fit the latest WHO criteria for PPL.
Results
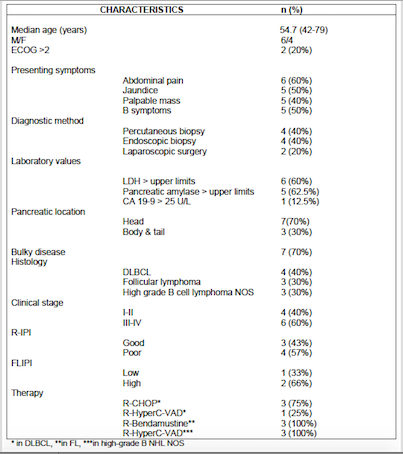
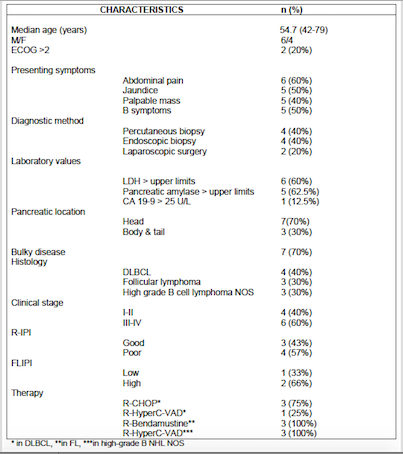
10 patients with PPL were identified: median age was 54 years, 6 patients were males. Clinical manifestations included abdominal pain, jaundice, a palpable epigastric mass and systemic symptoms. None of these patients had a history of previous pancreatitis, one had a positive serology for hepatitis B. Laboratory tests evidenced a normal hemogram in all cases, while LDH and pancreatic amylase were augmented in 6 and 5 patients, respectively. CA 19-9 was slightly increased in 1 patient only. The histopathological diagnosis was obtained by percutaneous or endoscopic biopsy or surgery and revealed: DLBCL (n=4), follicular lymphoma (FL) (n=3) and high-grade B-cell lymphomas not otherwise specified (n=3). In 7 cases PPL was bulky and occupied the pancreatic head. All patients underwent a first line immune-chemotherapy: R-Bendamustine (n=3), R-CHOP (n=3) or R-HyperC-VAD (n=4). Only 2 patients with a histopathologica diagnosis of FL achieved a complete remission (20%). The 7 patients with aggressive lymphoma had a median progression free survival of 4 months and an overall survival of 24 months.
Conclusion
PPL represents a rare and difficult-to-recognize disease. Most patients in our series complained symptoms characteristics of pancreatic adenocarcinoma such as abdominal pain, jaundice, and weight loss. However increased LDH serum levels and normal CA19-9 were associated to a diagnosis of NHL, as confirmed by histopathological analysis. The poor outcome of patients with high-grade PPL suggests the need of aggressive first-line immune-chemotherapy regimens, possibly followed by autologous stem cell transplantation. Obviously larger series of patients are awaited in order to drawn definitive conclusions on this rare extranodal NHL.
Session topic: 21. Aggressive Non-Hodgkin lymphoma - Clinical
Keyword(s): Clinical data, Extranodal lymphoma, Pancreas
Abstract: PB1773
Type: Publication Only
Background
Primary Pancreatic Lymphoma (PPL) is a very rare disease, representing only 0.1% of lymphomas and 0.2% of pancreatic tumors. According to the WHO classification the diagnostic criteria for PPL are: i) the bulk of the disease has to localize in the pancreas; ii) although adjacent and distant spread may be exist the primary clinical presentation has to involve the pancreatic gland. PPL presentation is variable and may overlap the onset of other neoplastic or inflammatory pancreatic diseases, often resulting in diagnostic difficulties. Histopathological examination usually reveals a diffuse large B cell lymphoma (DLBCL), nonetheless other types of lymphomas have been reported including the indolent ones. Diagnosis can be obtained through a percutaneous/endoscopic ultrasound-guided biopsy or surgery. An accurate histological characterization is essential because, unlike epithelial tumors, PPL does not benefit from surgery.
Aims
to evaluate retrospectively clinical, laboratory and histological characteristics, diagnosis, treatment, and outcome of a series of PPL patients diagnosed in 2 hematology units.
Methods
patients diagnosed with PPL between 2008 and 2017 were retrieved from the medical record databases of the Verona and Vicenza Hematology Units. Inclusion criteria were the availability of information related to clinical onset, histopathological diagnosis, laboratory tests, radiology imaging, treatment and follow-up. Patients with secondary pancreatic involvement of lymphoma were excluded. All cases herein presented were revised to ensure that they fit the latest WHO criteria for PPL.
Results
10 patients with PPL were identified: median age was 54 years, 6 patients were males. Clinical manifestations included abdominal pain, jaundice, a palpable epigastric mass and systemic symptoms. None of these patients had a history of previous pancreatitis, one had a positive serology for hepatitis B. Laboratory tests evidenced a normal hemogram in all cases, while LDH and pancreatic amylase were augmented in 6 and 5 patients, respectively. CA 19-9 was slightly increased in 1 patient only. The histopathological diagnosis was obtained by percutaneous or endoscopic biopsy or surgery and revealed: DLBCL (n=4), follicular lymphoma (FL) (n=3) and high-grade B-cell lymphomas not otherwise specified (n=3). In 7 cases PPL was bulky and occupied the pancreatic head. All patients underwent a first line immune-chemotherapy: R-Bendamustine (n=3), R-CHOP (n=3) or R-HyperC-VAD (n=4). Only 2 patients with a histopathologica diagnosis of FL achieved a complete remission (20%). The 7 patients with aggressive lymphoma had a median progression free survival of 4 months and an overall survival of 24 months.
Conclusion
PPL represents a rare and difficult-to-recognize disease. Most patients in our series complained symptoms characteristics of pancreatic adenocarcinoma such as abdominal pain, jaundice, and weight loss. However increased LDH serum levels and normal CA19-9 were associated to a diagnosis of NHL, as confirmed by histopathological analysis. The poor outcome of patients with high-grade PPL suggests the need of aggressive first-line immune-chemotherapy regimens, possibly followed by autologous stem cell transplantation. Obviously larger series of patients are awaited in order to drawn definitive conclusions on this rare extranodal NHL.
Session topic: 21. Aggressive Non-Hodgkin lymphoma - Clinical
Keyword(s): Clinical data, Extranodal lymphoma, Pancreas


