
Contributions
Abstract: PB1782
Type: Publication Only
Background
High-dose methotrexate (HDMTX) is an important component in the treatment protocols of certain hematological malignancies. A significant complication of this treatment is renal failure. There is paucity of data regarding the occurrence of acute kidney injury (AKI) following HDMTX in hemato-oncological patients. Herein we aimed to explore the incidence and risk factors of AKI after HDMTX therapy.
Aims
1. explore the incidence of AKI after HDMTX administration.
2. define the putative patients' baseline characteristics that predict the occurrence of AKI.
Methods
This is a single center, retrospective study. We reviewed the medical records of all consecutive patients who received a total MTX dose of 1500 mg or more. For these patients we collected demographic, clinical and outcome data. Acute kidney injury (AKI) was defined according to Acute Kidney Injury Network (AKIN) criteria (an increase in serum creatinine of at least 0.3 mg/dL). We compared patients with or without renal toxicity. For categorical variables, we used the χ2 test. We used a logistic regression model with the exp(β) as an estimator of the odds ratio and the confidence interval around it in order to define which baseline variables, predict renal toxicity. We used receiver operator characteristics (ROC) curves and the area under the curve to define the best cutoff for continuous variables. The probability of overall survival (OS) was estimated by the Kaplan-Meier method. The log-rank test was used to compare survival distributions.
Results
Between January 2012 and December 2016, 136 patients received at least one course of HDMTX in our Institute. Indications for HDMTX included: primary CNS lymphoma (n=12, 9%), other types of lymphoma (including as primary prophylaxis) (n= 96, 70%), acute lymphatic leukemia (n=24, 18%) or for various other diagnoses (n=4, 3%). The median age at diagnosis was 58 years (range 22 to 84), and 68 were males (50%). The vast majority were of good functional status, and 46 (34%) had at least one major comorbidity: vascular (n=18, 13%), diabetes (n=23, 17%) or prior malignancy (n=9, 7%) .
The median number of cycles per patient was 2 (range 1 to 10) and the median dose of MTX adjusted to body surface area (BSA) was 1670 mg/m2 (range: 743 to 3865 ).
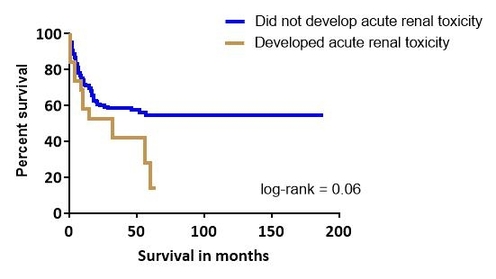
The median time until MTX clearance was 5 days (range 3 to 20). During this time AKI developed in 12% of patients (n=16). In a univariate analysis for prediction of acute nephrotoxicity: age above 58 years (p=0.03), LDH above 470 units/L (p=0.02), MTX dose adjusted for BSA above 1640 mg/m2 (p=0.015) and low levels of albumin at baseline (p=0.04) predicted acute MTX associated renal toxicity. In a multivariable analysis only age above 58 years remained predictive (Odds Ratio 4.6, 95% confidence interval 1.16-18.4). In 80% of cases, the creatinine levels returned to normal within 1 month. Yet, the median survival of patients who developed acute toxicity was only 38 months, while it was not reached in patients who maintained normal kidney function (Log rank= 0.06).
Conclusion
Older age is the strongest risk factor which predicts AKI in patients receiving HDMTX. While the rise in creatinine levels is usually reversible, AKI was associated with increased mortality rates. Whether decreasing the MTX doses in the elderly population will improve outcome in these patients warrants further investigation.
Session topic: 21. Aggressive Non-Hodgkin lymphoma - Clinical
Keyword(s): adult, CNS lymphoma, Methotrexate, Renal failure
Abstract: PB1782
Type: Publication Only
Background
High-dose methotrexate (HDMTX) is an important component in the treatment protocols of certain hematological malignancies. A significant complication of this treatment is renal failure. There is paucity of data regarding the occurrence of acute kidney injury (AKI) following HDMTX in hemato-oncological patients. Herein we aimed to explore the incidence and risk factors of AKI after HDMTX therapy.
Aims
1. explore the incidence of AKI after HDMTX administration.
2. define the putative patients' baseline characteristics that predict the occurrence of AKI.
Methods
This is a single center, retrospective study. We reviewed the medical records of all consecutive patients who received a total MTX dose of 1500 mg or more. For these patients we collected demographic, clinical and outcome data. Acute kidney injury (AKI) was defined according to Acute Kidney Injury Network (AKIN) criteria (an increase in serum creatinine of at least 0.3 mg/dL). We compared patients with or without renal toxicity. For categorical variables, we used the χ2 test. We used a logistic regression model with the exp(β) as an estimator of the odds ratio and the confidence interval around it in order to define which baseline variables, predict renal toxicity. We used receiver operator characteristics (ROC) curves and the area under the curve to define the best cutoff for continuous variables. The probability of overall survival (OS) was estimated by the Kaplan-Meier method. The log-rank test was used to compare survival distributions.
Results
Between January 2012 and December 2016, 136 patients received at least one course of HDMTX in our Institute. Indications for HDMTX included: primary CNS lymphoma (n=12, 9%), other types of lymphoma (including as primary prophylaxis) (n= 96, 70%), acute lymphatic leukemia (n=24, 18%) or for various other diagnoses (n=4, 3%). The median age at diagnosis was 58 years (range 22 to 84), and 68 were males (50%). The vast majority were of good functional status, and 46 (34%) had at least one major comorbidity: vascular (n=18, 13%), diabetes (n=23, 17%) or prior malignancy (n=9, 7%) .
The median number of cycles per patient was 2 (range 1 to 10) and the median dose of MTX adjusted to body surface area (BSA) was 1670 mg/m2 (range: 743 to 3865 ).
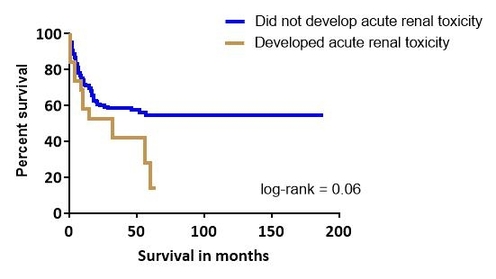
The median time until MTX clearance was 5 days (range 3 to 20). During this time AKI developed in 12% of patients (n=16). In a univariate analysis for prediction of acute nephrotoxicity: age above 58 years (p=0.03), LDH above 470 units/L (p=0.02), MTX dose adjusted for BSA above 1640 mg/m2 (p=0.015) and low levels of albumin at baseline (p=0.04) predicted acute MTX associated renal toxicity. In a multivariable analysis only age above 58 years remained predictive (Odds Ratio 4.6, 95% confidence interval 1.16-18.4). In 80% of cases, the creatinine levels returned to normal within 1 month. Yet, the median survival of patients who developed acute toxicity was only 38 months, while it was not reached in patients who maintained normal kidney function (Log rank= 0.06).
Conclusion
Older age is the strongest risk factor which predicts AKI in patients receiving HDMTX. While the rise in creatinine levels is usually reversible, AKI was associated with increased mortality rates. Whether decreasing the MTX doses in the elderly population will improve outcome in these patients warrants further investigation.
Session topic: 21. Aggressive Non-Hodgkin lymphoma - Clinical
Keyword(s): adult, CNS lymphoma, Methotrexate, Renal failure


