
Contributions
Abstract: PB1762
Type: Publication Only
Background
Neurological symptoms related to the involvement of the central nervous system have been commonly seen at diagnosis and at relapse in intravascular large B-cell lymphoma (IVLBCL). Although various patterns of abnormal findings on brain magnetic resonance imaging (MRI) in patients with IVLBCL have been reported, most of them were from case reports or small case series in selected patients.
Aims
We aimed to investigate the clinical value of abnormal findings detected by brain MRI in patients with IVLBCL with regard to diagnosis and prognosis.
Methods
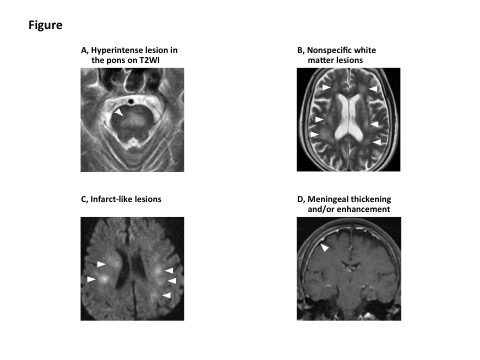
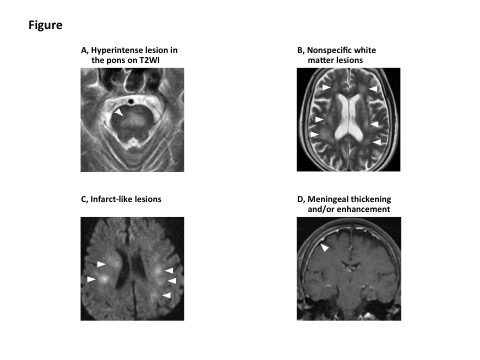
Thirty-three consecutive patients pathologically diagnosed and treated at Kameda Medical Center between 1998 and 2017 were identified. The baseline clinical characteristics, treatments, and outcomes of these 33 patients had been retrospectively reviewed. Brain MRI was performed as previously reported, and the abnormalities were classified into the following four patterns by two neuroradiologists (Figure): (1) hyperintense lesion in the pons on T2-weighted imaging (T2WI), (2) nonspecific white matter lesions, (3) infarct-like lesions, and (4) meningeal thickening and/or enhancement.
Results
We identified 18 patients with NL with a total of 53 involved peripheral nerves (PN) diagnosed and treated at our institution who were evaluated with both pretreatment contrast-enhanced MRI and PET-CT. Among the 18 patients with NL, contrast-enhanced MRI described abnormal findings on PN in 17 (94.4%) patients, while PET-CT described them in 12 (66.7%) patients, although the difference was slightly insignificant (P=0.074). Among the 53 involved PN, 52 (98.1%) were positive for contrast-enhanced MRI, while only 21 (39.6%) were positive for PET-CT (P<0.001). Detection sensitivities of PET-CT for cauda equine (11.1%) and lumbosacral nerves (31.0%) were lower compared to contrast-enhanced MRI, whereas PET-CT detected abnormal findings on cranial nerves with as high detection sensitivity (81.8%) as contrast-enhanced MRI. Patients who were negative for PET-CT included more patients with systemic presentation of lymphoma compared to those who were positive for PET-CT, although the difference was not statistically significant (50.0% vs. 33.3%, respectively; P=0.627), and soluble interleukin-2 receptor in patients with NL negative for PET-CT was significantly higher than those positive for PET-CT (P=0.049). Patients negative for PET-CT had relatively favorable overall survival than those positive for PET-CT (median, 37.2 vs. 7.5 months, respectively; P=0.234). All abnormal findings on PN described by contrast-enhanced MRI and PET-CT in patients who responded to therapy and had follow-up imaging studies showed significant improvement, suggesting that these findings were the manifestations of neural involvement of NL.
Conclusion
Our findings revealed that most patients with IVLBCL presented abnormal findings on pretreatment brain MRI even if they had no neurological symptom. In particular, hyperintense lesion in the pons on T2WI was frequently observed in patients with IVLBCL irrespective of presence or absence of impaired consciousness, suggesting that this pattern may be pathognomonic and valuable for timely diagnosis of IVLBCL. Improvement in all types of abnormal findings on follow-up brain MRI indicated that all these findings might reflect structural changes associated with IVLBCL and might be useful for confirmation of the therapeutic effect.
Session topic: 21. Aggressive Non-Hodgkin lymphoma - Clinical
Keyword(s): B cell lymphoma, Diagnosis, Magnetic resonance imaging
Abstract: PB1762
Type: Publication Only
Background
Neurological symptoms related to the involvement of the central nervous system have been commonly seen at diagnosis and at relapse in intravascular large B-cell lymphoma (IVLBCL). Although various patterns of abnormal findings on brain magnetic resonance imaging (MRI) in patients with IVLBCL have been reported, most of them were from case reports or small case series in selected patients.
Aims
We aimed to investigate the clinical value of abnormal findings detected by brain MRI in patients with IVLBCL with regard to diagnosis and prognosis.
Methods
Thirty-three consecutive patients pathologically diagnosed and treated at Kameda Medical Center between 1998 and 2017 were identified. The baseline clinical characteristics, treatments, and outcomes of these 33 patients had been retrospectively reviewed. Brain MRI was performed as previously reported, and the abnormalities were classified into the following four patterns by two neuroradiologists (Figure): (1) hyperintense lesion in the pons on T2-weighted imaging (T2WI), (2) nonspecific white matter lesions, (3) infarct-like lesions, and (4) meningeal thickening and/or enhancement.
Results
We identified 18 patients with NL with a total of 53 involved peripheral nerves (PN) diagnosed and treated at our institution who were evaluated with both pretreatment contrast-enhanced MRI and PET-CT. Among the 18 patients with NL, contrast-enhanced MRI described abnormal findings on PN in 17 (94.4%) patients, while PET-CT described them in 12 (66.7%) patients, although the difference was slightly insignificant (P=0.074). Among the 53 involved PN, 52 (98.1%) were positive for contrast-enhanced MRI, while only 21 (39.6%) were positive for PET-CT (P<0.001). Detection sensitivities of PET-CT for cauda equine (11.1%) and lumbosacral nerves (31.0%) were lower compared to contrast-enhanced MRI, whereas PET-CT detected abnormal findings on cranial nerves with as high detection sensitivity (81.8%) as contrast-enhanced MRI. Patients who were negative for PET-CT included more patients with systemic presentation of lymphoma compared to those who were positive for PET-CT, although the difference was not statistically significant (50.0% vs. 33.3%, respectively; P=0.627), and soluble interleukin-2 receptor in patients with NL negative for PET-CT was significantly higher than those positive for PET-CT (P=0.049). Patients negative for PET-CT had relatively favorable overall survival than those positive for PET-CT (median, 37.2 vs. 7.5 months, respectively; P=0.234). All abnormal findings on PN described by contrast-enhanced MRI and PET-CT in patients who responded to therapy and had follow-up imaging studies showed significant improvement, suggesting that these findings were the manifestations of neural involvement of NL.
Conclusion
Our findings revealed that most patients with IVLBCL presented abnormal findings on pretreatment brain MRI even if they had no neurological symptom. In particular, hyperintense lesion in the pons on T2WI was frequently observed in patients with IVLBCL irrespective of presence or absence of impaired consciousness, suggesting that this pattern may be pathognomonic and valuable for timely diagnosis of IVLBCL. Improvement in all types of abnormal findings on follow-up brain MRI indicated that all these findings might reflect structural changes associated with IVLBCL and might be useful for confirmation of the therapeutic effect.
Session topic: 21. Aggressive Non-Hodgkin lymphoma - Clinical
Keyword(s): B cell lymphoma, Diagnosis, Magnetic resonance imaging


