
Contributions
Abstract: PB1758
Type: Publication Only
Background
Primary central nervous system lymphoma (PCNSL) is a relatively rare nonHodgkin lymphoma (NHL) and counts for approximate 3% of all CNS neoplasms. Despite advances in treatment, patients still encounter early mortality. The previous reports focused on long-term outcomes (Abrey LE et al, J Clin Oncol, 2006; Ferreri AJ et al, J Clin Oncol, 2003), in which the risk factors included age, performance status, CSF protein level, involvement of deep brain, serum lactate dehydrogenase, and intraocular involvement.
Aims
In this study, we would like to investigate the risk factors of early mortality in patients with PCNSL.
Methods
We enrolled newly diagnosed PCNSL patients at Taipei Veterans General Hospital, a national medical center in Taiwan, between January 1, 2002 and October 31, 2017. Patients without histopathological confirmations, those diagnosed with secondary CNS lymphoma, or those with AIDS were excluded. The cohort was followed up until the end of February 2018. The risk factors for mortality within 180 days were identified using univariate and multivariate Cox proportional hazards models. The factors with p < 0.1 in the univariate analysis were included in the multivariate analysis. All treatments were estimated with the use of time-dependent covariates to prevent immortal time bias.
Results
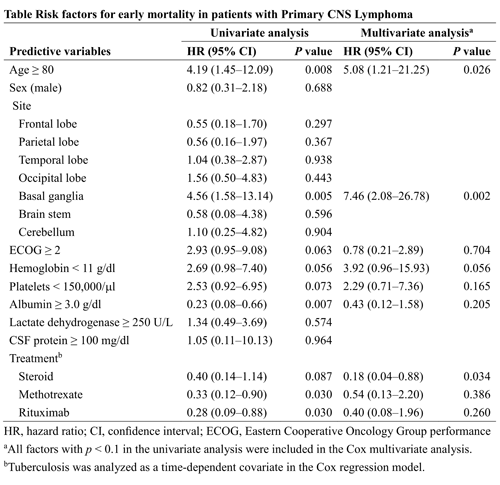
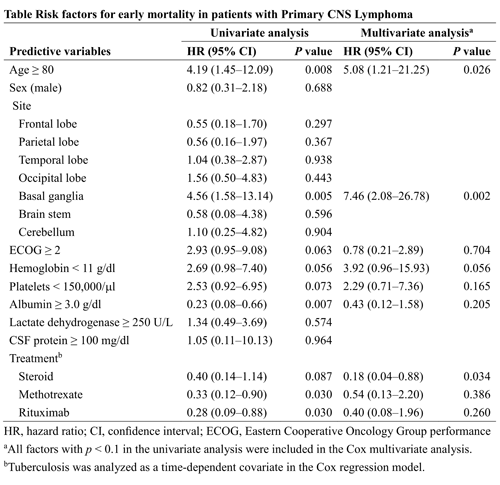
The study cohort consisted of 129 PCNSL patients, with a median follow-up of 8.4 years. The median age of the patients was 64 years and 73 (56.6%) of them were male. The probability of early mortality (≤ 180 days) was 13.4% (95% confidence interval [CI] 8.4–20.9%). In the univariate analysis, age ≥ 80 (hazards ratio [HR] 4.19), involvement of basal ganglia (HR 4.56) and ECOG performance status ≥ 2 (HR 2.93), hemoglobin < 11 g/dl (HR 2.69), platelets < 150,000/ml (HR 2.53), albumin ≥ 3.9 g/dl (HR 0.23), receiving steroid (HR 0.40), methotrexate (HR 0.33), and immunotherapy with rituximab (HR 0.28) were associated with early mortality. Age ≥ 80 (adjusted HR 5.08, 95% CI 1.21–21.25, p = 0.026), involvement of basal ganglia (adjusted HR 7.46, 95% CI 2.08–26.78, p = 0.002), and receiving steroid (adjusted HR 0.18, 95% CI 0.04–0.88, p = 0.034) were identified as independent predictors for early mortality in the multivariate analysis.
Conclusion
We identified age ≥ 80 and involvement of basal ganglia as independent risk factors for early mortality in the patients with PCNSL. Of note, steroid treatment could prevent the patients from the early death. Identifying patients with risks of early mortality may help clinicians initiate appropriate management and early treatment. Further validation of our findings in other cohorts is warranted.
Session topic: 21. Aggressive Non-Hodgkin lymphoma - Clinical
Keyword(s): CNS lymphoma, epidemiology, Mortality, Prognostic factor
Abstract: PB1758
Type: Publication Only
Background
Primary central nervous system lymphoma (PCNSL) is a relatively rare nonHodgkin lymphoma (NHL) and counts for approximate 3% of all CNS neoplasms. Despite advances in treatment, patients still encounter early mortality. The previous reports focused on long-term outcomes (Abrey LE et al, J Clin Oncol, 2006; Ferreri AJ et al, J Clin Oncol, 2003), in which the risk factors included age, performance status, CSF protein level, involvement of deep brain, serum lactate dehydrogenase, and intraocular involvement.
Aims
In this study, we would like to investigate the risk factors of early mortality in patients with PCNSL.
Methods
We enrolled newly diagnosed PCNSL patients at Taipei Veterans General Hospital, a national medical center in Taiwan, between January 1, 2002 and October 31, 2017. Patients without histopathological confirmations, those diagnosed with secondary CNS lymphoma, or those with AIDS were excluded. The cohort was followed up until the end of February 2018. The risk factors for mortality within 180 days were identified using univariate and multivariate Cox proportional hazards models. The factors with p < 0.1 in the univariate analysis were included in the multivariate analysis. All treatments were estimated with the use of time-dependent covariates to prevent immortal time bias.
Results
The study cohort consisted of 129 PCNSL patients, with a median follow-up of 8.4 years. The median age of the patients was 64 years and 73 (56.6%) of them were male. The probability of early mortality (≤ 180 days) was 13.4% (95% confidence interval [CI] 8.4–20.9%). In the univariate analysis, age ≥ 80 (hazards ratio [HR] 4.19), involvement of basal ganglia (HR 4.56) and ECOG performance status ≥ 2 (HR 2.93), hemoglobin < 11 g/dl (HR 2.69), platelets < 150,000/ml (HR 2.53), albumin ≥ 3.9 g/dl (HR 0.23), receiving steroid (HR 0.40), methotrexate (HR 0.33), and immunotherapy with rituximab (HR 0.28) were associated with early mortality. Age ≥ 80 (adjusted HR 5.08, 95% CI 1.21–21.25, p = 0.026), involvement of basal ganglia (adjusted HR 7.46, 95% CI 2.08–26.78, p = 0.002), and receiving steroid (adjusted HR 0.18, 95% CI 0.04–0.88, p = 0.034) were identified as independent predictors for early mortality in the multivariate analysis.
Conclusion
We identified age ≥ 80 and involvement of basal ganglia as independent risk factors for early mortality in the patients with PCNSL. Of note, steroid treatment could prevent the patients from the early death. Identifying patients with risks of early mortality may help clinicians initiate appropriate management and early treatment. Further validation of our findings in other cohorts is warranted.
Session topic: 21. Aggressive Non-Hodgkin lymphoma - Clinical
Keyword(s): CNS lymphoma, epidemiology, Mortality, Prognostic factor


