
Contributions
Abstract: PB1764
Type: Publication Only
Background
Diffuse large B cell lymphoma (DLBCL) is diagnosed in 3-5/100,000 people annually, with RCHOP (Rituximab, Cyclophosphamide, Hydroxydaunorubicin, Oncovin, and Prednisolone) chemotherapy remaining the standard & central nervous system (CNS) prophylaxis delivered based on an International Prognostic Index (IPI) of 4/5, or having a high risk anatomical site. Extended molecular histopathology with Ki67 proliferative index, cell of origin immunohistochemistry (COO-IHC: germinal centre/GCB or activated B cell/ABC), MYC expression, & genetic rearrangements are now routinely undertaken to evaluate prognosis. Local audit of practice is essential to capture histopathological diversity, early response, & mortality rates to ensure that we can adapt and provide the best care possible.
Aims
This retrospective audit scrutinises diagnostics, initial therapy, & mortality of DLBCL treated at a busy general hospital serving 800,000 people in a socio-economically challenged area of London, UK.
Methods
100 patients diagnosed in 2016 & 2017 were retrospectively assessed using electronic health records. The Swedish Lymphoma Registry (SLR) was chosen as a comparator dataset.
Results
To obtain a snapshot of diagnostics and initial care, median follow-up was short (150 days). Median age was 72 years (27-90, where 33% of patients were over 80). 65% presented with stage 3/4 disease (comparable with SLR). IPI was 4 or 5 in 43% of patients (16% in SLR). 60% of patients were initiated on RCHOP chemotherapy and 20% on RCVP or R-Gem-CVP due to comorbidities. 2 received RCODOX-M due to high risk features. 15% received only palliative steroids or radiotherapy. CNS prophylaxis criteria were met in 50% of cases: 90% due to high IPI; 10% due to anatomical site. Prophylaxis was only administered in 15% of these cases (IT methotrexate alone in 50% & systemic methotrexate in 50%). Omissions were due to patients being unfit for treatment. 4 CNS relapses occured with 2 deemed high risk at diagnosis.
Of the 85% of biopsies reporting Ki-67, 60% had a Ki-67>90% (10-30% reported elsewhere). COO-IHC was ABC in 41% of cases, GCB in 30%, & unclassifiable in 35% (comparable to literature). Of the 90% of cases reporting MYC, 44% showed overexpression where 85% were double or triple expresser with BCL2/6. Rearrangement of MYC/BCL2/BCL6 genes were assessed by FISH in only 45% of cases (45% omitted due to low IHC MYC expression, 30% due to inadequate biopsy material). In the 37 cases assessed, 5% showed only MYC rearrangement & 15% had a double or triple hit, greater than the rates of 5-10% reported elsewhere.
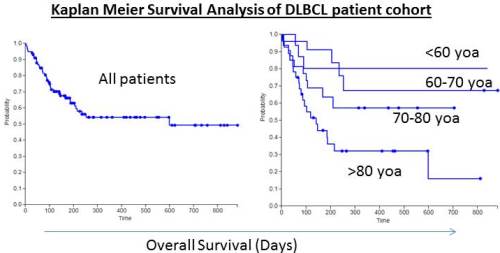
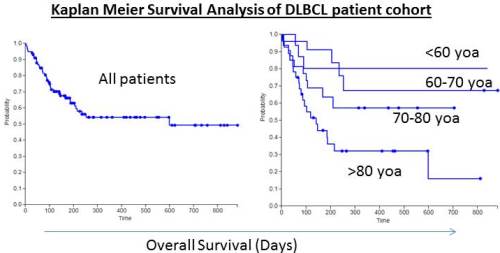
Around 80% of patients under 60 years of age(yoa), 70% of patients 60-70yoa, & 60% of patients 70-80yoa survive 2 years, comparable to the SLR. 23 patients died within 100 days of diagnosis of whom 13 were over 80yoa & 3 under 60yoa. 62% of patients diagnosed over 80yoa died within 100 days; 50% of these deaths occurred in palliative patients & 50% received chemotherapy.
Conclusion
This audit has revealed survival rates largely comparable to the registry data, but with high early death rates requiring scrutiny. High IPI scores account for a greater proportion than expected (43% vs 16% in the SLR). This may reflect late presentation of disease, or more molecular adverse features, with Ki67>90% & ‘double-hit’ disease apparently over-represented in this cohort. We emphasise that audit of ‘real-world’ practice is essential to elicit trends & regional differences, ensure equitable high quality care & delivery, enabling tailored service provision to its population.
Session topic: 21. Aggressive Non-Hodgkin lymphoma - Clinical
Keyword(s): DLBCL, International prognostic index, Ki-67, Mortality
Abstract: PB1764
Type: Publication Only
Background
Diffuse large B cell lymphoma (DLBCL) is diagnosed in 3-5/100,000 people annually, with RCHOP (Rituximab, Cyclophosphamide, Hydroxydaunorubicin, Oncovin, and Prednisolone) chemotherapy remaining the standard & central nervous system (CNS) prophylaxis delivered based on an International Prognostic Index (IPI) of 4/5, or having a high risk anatomical site. Extended molecular histopathology with Ki67 proliferative index, cell of origin immunohistochemistry (COO-IHC: germinal centre/GCB or activated B cell/ABC), MYC expression, & genetic rearrangements are now routinely undertaken to evaluate prognosis. Local audit of practice is essential to capture histopathological diversity, early response, & mortality rates to ensure that we can adapt and provide the best care possible.
Aims
This retrospective audit scrutinises diagnostics, initial therapy, & mortality of DLBCL treated at a busy general hospital serving 800,000 people in a socio-economically challenged area of London, UK.
Methods
100 patients diagnosed in 2016 & 2017 were retrospectively assessed using electronic health records. The Swedish Lymphoma Registry (SLR) was chosen as a comparator dataset.
Results
To obtain a snapshot of diagnostics and initial care, median follow-up was short (150 days). Median age was 72 years (27-90, where 33% of patients were over 80). 65% presented with stage 3/4 disease (comparable with SLR). IPI was 4 or 5 in 43% of patients (16% in SLR). 60% of patients were initiated on RCHOP chemotherapy and 20% on RCVP or R-Gem-CVP due to comorbidities. 2 received RCODOX-M due to high risk features. 15% received only palliative steroids or radiotherapy. CNS prophylaxis criteria were met in 50% of cases: 90% due to high IPI; 10% due to anatomical site. Prophylaxis was only administered in 15% of these cases (IT methotrexate alone in 50% & systemic methotrexate in 50%). Omissions were due to patients being unfit for treatment. 4 CNS relapses occured with 2 deemed high risk at diagnosis.
Of the 85% of biopsies reporting Ki-67, 60% had a Ki-67>90% (10-30% reported elsewhere). COO-IHC was ABC in 41% of cases, GCB in 30%, & unclassifiable in 35% (comparable to literature). Of the 90% of cases reporting MYC, 44% showed overexpression where 85% were double or triple expresser with BCL2/6. Rearrangement of MYC/BCL2/BCL6 genes were assessed by FISH in only 45% of cases (45% omitted due to low IHC MYC expression, 30% due to inadequate biopsy material). In the 37 cases assessed, 5% showed only MYC rearrangement & 15% had a double or triple hit, greater than the rates of 5-10% reported elsewhere.
Around 80% of patients under 60 years of age(yoa), 70% of patients 60-70yoa, & 60% of patients 70-80yoa survive 2 years, comparable to the SLR. 23 patients died within 100 days of diagnosis of whom 13 were over 80yoa & 3 under 60yoa. 62% of patients diagnosed over 80yoa died within 100 days; 50% of these deaths occurred in palliative patients & 50% received chemotherapy.
Conclusion
This audit has revealed survival rates largely comparable to the registry data, but with high early death rates requiring scrutiny. High IPI scores account for a greater proportion than expected (43% vs 16% in the SLR). This may reflect late presentation of disease, or more molecular adverse features, with Ki67>90% & ‘double-hit’ disease apparently over-represented in this cohort. We emphasise that audit of ‘real-world’ practice is essential to elicit trends & regional differences, ensure equitable high quality care & delivery, enabling tailored service provision to its population.
Session topic: 21. Aggressive Non-Hodgkin lymphoma - Clinical
Keyword(s): DLBCL, International prognostic index, Ki-67, Mortality


