
Contributions
Abstract: PB1753
Type: Publication Only
Background
Neurolymphomatosis (NL) is an extremely rare clinical condition and its optimal diagnostic approach remains unclear. Although pathological confirmation is the gold standard for NL diagnosis, it is often unfeasible due to the anatomical difficulty in approaching the culprit lesions and the potential risk of irreversible nerve damage caused by nerve biopsy. Contrast-enhanced magnetic resonance imaging (MRI) and fluorine-18 fluorodeoxyglucose (18-FDG) positron emission tomography-computed tomography (PET-CT) have been identified as useful modalities for the NL diagnosis. However, the sensitivities of contrast-enhanced (MRI) and 18F-FDG PET-CT have not been compared thus far.
Aims
We aimed to compare the usefulness and detection sensitivities of contrast-enhanced MRI and PET-CT for the diagnosis of NL.
Methods
We enrolled 18 consecutive patients diagnosed with NL between 2007 and 2018. Criteria for diagnosis of NL were as follows: (1) clinical symptoms and/or neurological findings related to the peripheral nerves, and (2) histological confirmation of lymphoma cells within the peripheral nerves or imaging findings including enlargement and/or enhancement of these nerves detected by contrast-enhanced MRI and/or abnormal accumulation of 18F-FDG in these nerves detected by PET-CT. Imaging findings of all patients were confirmed by two experienced radiologists. Detection sensitivities were compared using the McNemar test.
Results
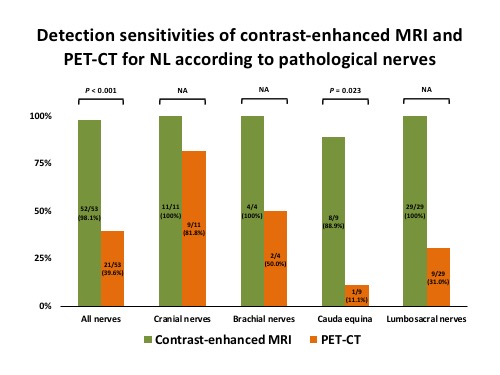
A total of 18 patients were treated at our institution and evaluated using both pretreatment contrast-enhanced MRI and PET-CT. Of these patients, contrast-enhanced MRI identified abnormal findings in 17 (94.4%) patients, while PET-CT identified them in 12 (66.7%) patients, although the difference was slightly insignificant (P = 0.074). Among the 53 involved PN, 52 (98.1%) were deemed positive for NL by contrast-enhanced MRI, whereas only 21 (39.6%) were deemed positive by PET-CT (P < 0.001). Detection sensitivity of PET-CT for the cauda equine (11.1%) and lumbosacral nerves (31.0%) was lower than that of contrast-enhanced MRI. However, PET-CT and contrast-enhanced MRI showed equivalent sensitivity for detection of abnormal findings in cranial nerves (81.8%). Levels of soluble interleukin-2 receptor in patients with NL who were deemed negative for NL by PET-CT were significantly higher than in those deemed positive for NL (P = 0.049). The group deemed negative for NL by PET-CT included more patients with systemic presentation of lymphoma than those deemed positive for NL by PET-CT, although the difference was not statistically significant (50.0% vs. 33.3%, respectively; P = 0.627). Additionally, patients deemed negative for NL by PET-CT had a more favorable overall survival than those deemed positive for NL (median, 37.2 vs. 7.5 months, respectively; P = 0.234). All abnormal findings for PN identified by contrast-enhanced and PET-CT in patients who responded to therapy and had follow-up imaging studies showed significant improvement, suggesting that these findings were the manifestations of neural involvements of NL.
Conclusion
To our knowledge, this is the first study to investigate the difference between detection sensitivities of contrast-enhancement MRI and PET-CT for the diagnosis of NL. Contrast-enhanced MRI has superior sensitivity to PET-CT for the diagnosis of NL, particularly in the cauda equine and lumbosacral nerves. Thus, contrast-enhanced MRI should be performed in combination with PET-CT for the diagnosis of NL.
Session topic: 21. Aggressive Non-Hodgkin lymphoma - Clinical
Keyword(s): B cell lymphoma, Diagnosis, MRI, PET
Abstract: PB1753
Type: Publication Only
Background
Neurolymphomatosis (NL) is an extremely rare clinical condition and its optimal diagnostic approach remains unclear. Although pathological confirmation is the gold standard for NL diagnosis, it is often unfeasible due to the anatomical difficulty in approaching the culprit lesions and the potential risk of irreversible nerve damage caused by nerve biopsy. Contrast-enhanced magnetic resonance imaging (MRI) and fluorine-18 fluorodeoxyglucose (18-FDG) positron emission tomography-computed tomography (PET-CT) have been identified as useful modalities for the NL diagnosis. However, the sensitivities of contrast-enhanced (MRI) and 18F-FDG PET-CT have not been compared thus far.
Aims
We aimed to compare the usefulness and detection sensitivities of contrast-enhanced MRI and PET-CT for the diagnosis of NL.
Methods
We enrolled 18 consecutive patients diagnosed with NL between 2007 and 2018. Criteria for diagnosis of NL were as follows: (1) clinical symptoms and/or neurological findings related to the peripheral nerves, and (2) histological confirmation of lymphoma cells within the peripheral nerves or imaging findings including enlargement and/or enhancement of these nerves detected by contrast-enhanced MRI and/or abnormal accumulation of 18F-FDG in these nerves detected by PET-CT. Imaging findings of all patients were confirmed by two experienced radiologists. Detection sensitivities were compared using the McNemar test.
Results
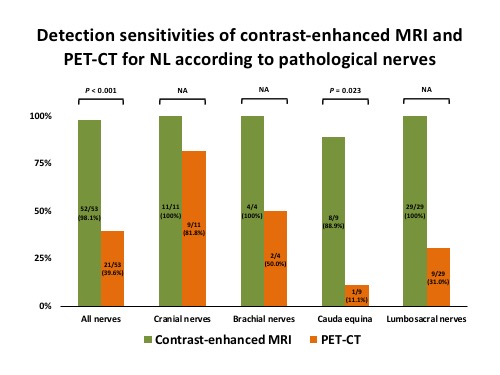
A total of 18 patients were treated at our institution and evaluated using both pretreatment contrast-enhanced MRI and PET-CT. Of these patients, contrast-enhanced MRI identified abnormal findings in 17 (94.4%) patients, while PET-CT identified them in 12 (66.7%) patients, although the difference was slightly insignificant (P = 0.074). Among the 53 involved PN, 52 (98.1%) were deemed positive for NL by contrast-enhanced MRI, whereas only 21 (39.6%) were deemed positive by PET-CT (P < 0.001). Detection sensitivity of PET-CT for the cauda equine (11.1%) and lumbosacral nerves (31.0%) was lower than that of contrast-enhanced MRI. However, PET-CT and contrast-enhanced MRI showed equivalent sensitivity for detection of abnormal findings in cranial nerves (81.8%). Levels of soluble interleukin-2 receptor in patients with NL who were deemed negative for NL by PET-CT were significantly higher than in those deemed positive for NL (P = 0.049). The group deemed negative for NL by PET-CT included more patients with systemic presentation of lymphoma than those deemed positive for NL by PET-CT, although the difference was not statistically significant (50.0% vs. 33.3%, respectively; P = 0.627). Additionally, patients deemed negative for NL by PET-CT had a more favorable overall survival than those deemed positive for NL (median, 37.2 vs. 7.5 months, respectively; P = 0.234). All abnormal findings for PN identified by contrast-enhanced and PET-CT in patients who responded to therapy and had follow-up imaging studies showed significant improvement, suggesting that these findings were the manifestations of neural involvements of NL.
Conclusion
To our knowledge, this is the first study to investigate the difference between detection sensitivities of contrast-enhancement MRI and PET-CT for the diagnosis of NL. Contrast-enhanced MRI has superior sensitivity to PET-CT for the diagnosis of NL, particularly in the cauda equine and lumbosacral nerves. Thus, contrast-enhanced MRI should be performed in combination with PET-CT for the diagnosis of NL.
Session topic: 21. Aggressive Non-Hodgkin lymphoma - Clinical
Keyword(s): B cell lymphoma, Diagnosis, MRI, PET


