
Contributions
Abstract: PB1785
Type: Publication Only
Background
ASCT is a cornerstone in lymphoma therapeutics, especially in the relapse setting. BEAM (Carmustine, Etoposide, Cytarabine and Melphalan) conditioning regimen is the most widely used with a low toxic mortality rate. Bendamustine has been occasionally used as a substitute for Carmustine (“BendaEAM”) during shortage periods. VOD is a potentially life-threatening complication, rarely observed after ASCT.
Aims
During the last 2 years, we observed 5 cases in patients treated with BEAM or BendaEAM in our department. Two patients required hepatic transplantation (HT).
Methods
We recorded cases of VOD observed in our department after ASCT. The new EBMT classification for VOD was used [1].
Results
Case 1 : A 54 y.o. woman was diagnosed in 2010 with grade I-II follicular lymphoma. Complete remission (CR) was obtained after 6 cycles of R-CHOP21 and 2 years of Rituximab maintenance. Upon relapse in March 2015, a second CR was obtained after 4 cycles of R-DHAOX (Rituximab, Dexamethasone, High-dose Cytarabine, Oxaliplatin) delivered every 3 weeks [2]. ASCT was performed in the setting of the “BENEFIT” study (NCT02008006) using BendaEAM with Bendamustine 200 mg/m². VOD started at day 5 with ascites, painful hepatomegaly, weight gain (11%) and jaundice. Factor V dropped and hepatic encephalopathy occurred. At day 15, HT permitted recovery. At 29 months of follow-up, she is in persisting CR and didn’t present any major complication of HT.
Case 2 : A 60 y.o. man was diagnosed in 2015 of diffuse large B-cell lymphoma treated by 8 cycles of R-CHOP. In May 2017, relapse occurred. Second CR was obtained with 3 cycles of R-DHAOX + Ibrutinib in the setting of the “BIBLOS” study (NCT02055924) followed by BEAM/ASCT. VOD started at day 8 with ascites, tender hepatomegaly, weight gain (8%) and jaundice. Low factor V and encephalopathy led the patient to receive an HT at day 12. After transient improvement, he died of septic choc.
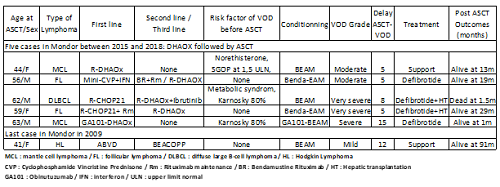
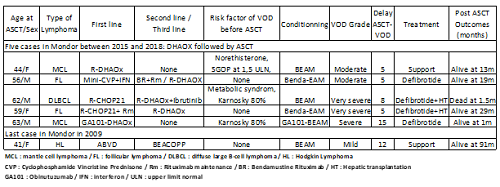
The same pattern was observed in 5 cases of VOD in last 3 years : R-DHAOx inductive salvage regimen followed by consolidative ASCT (conditioning by BEAM or BendaEAM). The last case before this period was a woman in 2009 who presented mild VOD after BEACOPP and BEAM/ASCT. Characteristics of these patients are described in table 1. None had major comorbidities. Between 2008 and 2017, incidence of VOD in our department following DHAOX/ASCT was 6.4 % (5/78) versus 1.3 % (1/75) after other salvage regimen/ASCT for lymphoma.
Conclusion
In the last decade, Cisplatin was often replaced by Oxaliplatin in the DHAP protocol in order to avoid renal impairment. Pre-operative Oxaliplatin in hepatic metastatic of colorectal cancer leads to asymptomatic sinusoidal damage in half of patients and could explain the increase of VOD in ASCT [3]. We need to be more aware of risk in this setting and national report is ongoing. Management of VOD could include HT with limits about status of disease and multi-organ failure.
Bibliography
1. Mohty M.Bone Marrow Transplant 2016;51(7):906–912.
2. Lignon J. Clin Lymphoma Myeloma Leuk 2010;10(4):262–269.
3. Rubbia-Brandt L. Ann Oncol 2004;15(3):460–466.
Session topic: 21. Aggressive Non-Hodgkin lymphoma - Clinical
Keyword(s): Autologous bone marrow transplant, lymphoma, Oxaliplatin, VOD
Abstract: PB1785
Type: Publication Only
Background
ASCT is a cornerstone in lymphoma therapeutics, especially in the relapse setting. BEAM (Carmustine, Etoposide, Cytarabine and Melphalan) conditioning regimen is the most widely used with a low toxic mortality rate. Bendamustine has been occasionally used as a substitute for Carmustine (“BendaEAM”) during shortage periods. VOD is a potentially life-threatening complication, rarely observed after ASCT.
Aims
During the last 2 years, we observed 5 cases in patients treated with BEAM or BendaEAM in our department. Two patients required hepatic transplantation (HT).
Methods
We recorded cases of VOD observed in our department after ASCT. The new EBMT classification for VOD was used [1].
Results
Case 1 : A 54 y.o. woman was diagnosed in 2010 with grade I-II follicular lymphoma. Complete remission (CR) was obtained after 6 cycles of R-CHOP21 and 2 years of Rituximab maintenance. Upon relapse in March 2015, a second CR was obtained after 4 cycles of R-DHAOX (Rituximab, Dexamethasone, High-dose Cytarabine, Oxaliplatin) delivered every 3 weeks [2]. ASCT was performed in the setting of the “BENEFIT” study (NCT02008006) using BendaEAM with Bendamustine 200 mg/m². VOD started at day 5 with ascites, painful hepatomegaly, weight gain (11%) and jaundice. Factor V dropped and hepatic encephalopathy occurred. At day 15, HT permitted recovery. At 29 months of follow-up, she is in persisting CR and didn’t present any major complication of HT.
Case 2 : A 60 y.o. man was diagnosed in 2015 of diffuse large B-cell lymphoma treated by 8 cycles of R-CHOP. In May 2017, relapse occurred. Second CR was obtained with 3 cycles of R-DHAOX + Ibrutinib in the setting of the “BIBLOS” study (NCT02055924) followed by BEAM/ASCT. VOD started at day 8 with ascites, tender hepatomegaly, weight gain (8%) and jaundice. Low factor V and encephalopathy led the patient to receive an HT at day 12. After transient improvement, he died of septic choc.
The same pattern was observed in 5 cases of VOD in last 3 years : R-DHAOx inductive salvage regimen followed by consolidative ASCT (conditioning by BEAM or BendaEAM). The last case before this period was a woman in 2009 who presented mild VOD after BEACOPP and BEAM/ASCT. Characteristics of these patients are described in table 1. None had major comorbidities. Between 2008 and 2017, incidence of VOD in our department following DHAOX/ASCT was 6.4 % (5/78) versus 1.3 % (1/75) after other salvage regimen/ASCT for lymphoma.
Conclusion
In the last decade, Cisplatin was often replaced by Oxaliplatin in the DHAP protocol in order to avoid renal impairment. Pre-operative Oxaliplatin in hepatic metastatic of colorectal cancer leads to asymptomatic sinusoidal damage in half of patients and could explain the increase of VOD in ASCT [3]. We need to be more aware of risk in this setting and national report is ongoing. Management of VOD could include HT with limits about status of disease and multi-organ failure.
Bibliography
1. Mohty M.Bone Marrow Transplant 2016;51(7):906–912.
2. Lignon J. Clin Lymphoma Myeloma Leuk 2010;10(4):262–269.
3. Rubbia-Brandt L. Ann Oncol 2004;15(3):460–466.
Session topic: 21. Aggressive Non-Hodgkin lymphoma - Clinical
Keyword(s): Autologous bone marrow transplant, lymphoma, Oxaliplatin, VOD


