
Contributions
Abstract: PB2013
Type: Publication Only
Background
Hodgkin lymphoma (HL) is a lymphoproliferative malignancy that represents approximately 10% of all cases of lymphoma. More than 90% of patients with favorable disease and 70-80% of patients with unfavorable disease are cured with an initial therapy that consists, above all, in two to four cicles of Doxorubicin, Bleomicin, Vinblastine and Dacarbazine (ABVD) for favorable disease or four to six cycles of ABVD for unfavorable disease, with or without radiotherapy. Late therapy-related effects in HL survivors include hypothyroidism, fertility issues, secondary cancers and vascular disease. Second malignancy was first recognized as a problem in the early 1970s. Increasing attention has focused on the more common individual tumor types, including lung cancer and breast cancer. The risk of secondary breast cancers is associated with young age in woman (particularly <30 years) and young age at the time of radiation. In the other hand, it is described that lung cancer risk is increased in who received mediastinal radiation and particularly in smokers.
Aims
We aim to evaluate the risk factors that increase the incidence of secondary malignances in patients con HL treated with ABVD +/- radiotherapy.
Methods
We retrospectively selected from the pathology registries of Son Llatzer Hospital (HSLL) patients with HL treated with ABVD +/- RT. Kaplan–Meier was used for time-to-event variables and the log-rank test was used to compare groups as well as Cox Regression for multivariate survival analysis.
Results
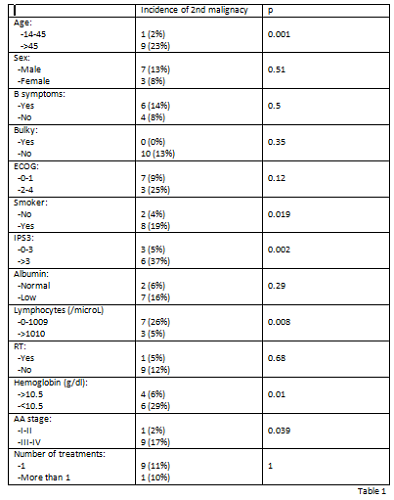
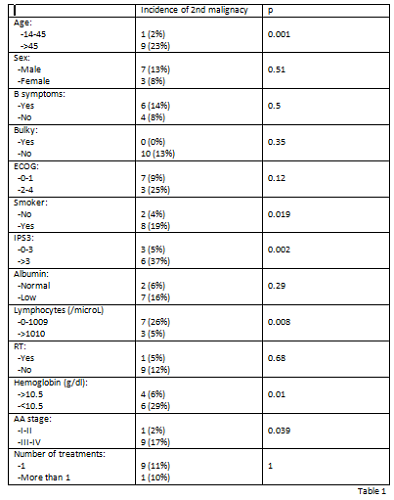
From 2001 to 2017, 94 patients fulfilled inclusion criteria. Median age was 42 years (14-84), 41% with >45 years, 58% males, 53% AA (Ann Arbor stage II-IV), 13% with ECOG performance status >1, 20% with IPS >3, 13% with low lymphocytes (<8% or <600/mm3. Response was as follows: 77 (82%) achieved complete response (CR), 5 (5%) partial response and 8 (8%) progression. 86% of global survival at 5 years and 82% of progression free survival at 5 years. With a median follow-up of 65 months, 10 second cancers and one concomitant malignancy were diagnosed in 94 patients: 7 respiratory tract malignancies, 2 gynecological cancers and 1 digestive tract cancer. The concomitant cancer was a breast cancer. Different factors at the time of diagnosis were associated in our patients with an increased incidence of secondary malignances. Univariate analysis showed that age >45 years, being smoker, IPS>3, low lymphocytes and advanced stage (III-IV) increased significantly the risk of secondary neoplasms (Table I). Multivariate analysis showed that only having >45 years (relative risk 14; 95 percent confidence interval, 1.6-125.9), lymphocytes <1010/mm3 (relative risk 6.4; 95 percent confidence interval, 1.3-31.7) and being smoker (relative risk 4.1; 95 percent confidence interval, 0.7-24.2) retained independent significance.
The number of cycles of ABVD received and the radiotherapy were not related with an increased incidence of secondary malignancies.
Conclusion
Patients with risk factors at diagnosis such as: smoking history, low lymphocytes and <45 years had an increased incidence of secondary neoplasms during the next years after ABVD. We conclude that it is important to emphasize, in this type of patients, the establishment of optimal prophylactic and screening strategies.
Session topic: 17. Hodgkin lymphoma – Clinical
Keyword(s): Hodgkin's Lymphoma, Second malignancy
Abstract: PB2013
Type: Publication Only
Background
Hodgkin lymphoma (HL) is a lymphoproliferative malignancy that represents approximately 10% of all cases of lymphoma. More than 90% of patients with favorable disease and 70-80% of patients with unfavorable disease are cured with an initial therapy that consists, above all, in two to four cicles of Doxorubicin, Bleomicin, Vinblastine and Dacarbazine (ABVD) for favorable disease or four to six cycles of ABVD for unfavorable disease, with or without radiotherapy. Late therapy-related effects in HL survivors include hypothyroidism, fertility issues, secondary cancers and vascular disease. Second malignancy was first recognized as a problem in the early 1970s. Increasing attention has focused on the more common individual tumor types, including lung cancer and breast cancer. The risk of secondary breast cancers is associated with young age in woman (particularly <30 years) and young age at the time of radiation. In the other hand, it is described that lung cancer risk is increased in who received mediastinal radiation and particularly in smokers.
Aims
We aim to evaluate the risk factors that increase the incidence of secondary malignances in patients con HL treated with ABVD +/- radiotherapy.
Methods
We retrospectively selected from the pathology registries of Son Llatzer Hospital (HSLL) patients with HL treated with ABVD +/- RT. Kaplan–Meier was used for time-to-event variables and the log-rank test was used to compare groups as well as Cox Regression for multivariate survival analysis.
Results
From 2001 to 2017, 94 patients fulfilled inclusion criteria. Median age was 42 years (14-84), 41% with >45 years, 58% males, 53% AA (Ann Arbor stage II-IV), 13% with ECOG performance status >1, 20% with IPS >3, 13% with low lymphocytes (<8% or <600/mm3. Response was as follows: 77 (82%) achieved complete response (CR), 5 (5%) partial response and 8 (8%) progression. 86% of global survival at 5 years and 82% of progression free survival at 5 years. With a median follow-up of 65 months, 10 second cancers and one concomitant malignancy were diagnosed in 94 patients: 7 respiratory tract malignancies, 2 gynecological cancers and 1 digestive tract cancer. The concomitant cancer was a breast cancer. Different factors at the time of diagnosis were associated in our patients with an increased incidence of secondary malignances. Univariate analysis showed that age >45 years, being smoker, IPS>3, low lymphocytes and advanced stage (III-IV) increased significantly the risk of secondary neoplasms (Table I). Multivariate analysis showed that only having >45 years (relative risk 14; 95 percent confidence interval, 1.6-125.9), lymphocytes <1010/mm3 (relative risk 6.4; 95 percent confidence interval, 1.3-31.7) and being smoker (relative risk 4.1; 95 percent confidence interval, 0.7-24.2) retained independent significance.
The number of cycles of ABVD received and the radiotherapy were not related with an increased incidence of secondary malignancies.
Conclusion
Patients with risk factors at diagnosis such as: smoking history, low lymphocytes and <45 years had an increased incidence of secondary neoplasms during the next years after ABVD. We conclude that it is important to emphasize, in this type of patients, the establishment of optimal prophylactic and screening strategies.
Session topic: 17. Hodgkin lymphoma – Clinical
Keyword(s): Hodgkin's Lymphoma, Second malignancy


