
Contributions
Abstract: PB2315
Type: Publication Only
Background
Systemic mastocytosis with an associated hematological neoplasm (SM-AHN) is the second most common subtype of SM (estimated frequency 21-44%). In the majority of patients with SM-AHN, a myeloid stem cell malignancy is diagnosed but association of essential thrombocythemia (ET) and SM is anecdotal
Aims
In this work we described a case of Essential Thrmobocythemia associated with Mastocytosis completely diagnosed according to the more recent WHO 2016 criteria and we performed a review of all reported cases in literature about this association.
Methods
We describe a 62 years-old man with thrombocytosis (600-750 x 10^9/L), longstanding hepato-splenomegaly and skin lesions compatible with maculopapular lesions at arms and legs roots (urticaria pigmentosa) treated with phototherapy. The patient had no lymphadenopathy. An abdomen ultrasound revealed fatty liver and splenomegaly (largest dimension 18.7 cm); in addition, lateral X-ray pictures of the thoraco-lumbar spine showed multiple moderate vertebral fractures. Hemoglobin and white cells count were normal; despite a normal ferritin, homozygosity for HFE H63D mutation was detected. We searched for and found JAK2V617F mutation (allele burden 9.3%). The bone marrow (BM) biopsy, showing normal cellularity with normal M:E ratio (3:1), preserved myeloid and erythroid maturation, increased megakaryopoiesis (6-7 megakaryocytes/HPF), large/giant megakaryocytes with hypersegmented nuclei disposed in loose clusters, confirmed the hypothesis of ET. Perivascular and paratrabecular aggregates of spindle-shaped mast cells (MCs) were also present. These cells featured fine metachromatic granules and were intermingled with eosinophils and mature-looking lymphocytes. By immunohistochemistry, MCs were positive for triptase and CD117, with aberrant expression of CD25 and CD2. An increase in bone marrow reticulin fibers (MF grade 2) was present in MC-infiltrated areas. Cytogenetic analysis disclosed a normal male karyotype (46, XY). Elevated serum triptase level (123 ng/mL) and oncogenic KIT D816V mutation definitely established the diagnosis of SM. No mutation in TET2, ASXL1, SRSF2, RUNX1 and CBL genes was found. Treatment with low-dose Aspirin and Hydroxycarbamide (HU) was started and the platelets count rapidly falls to normal values. Two years after diagnosis our patient is alive and in good clinical conditions.
Results
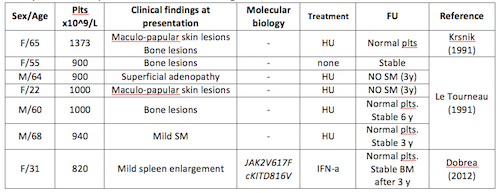
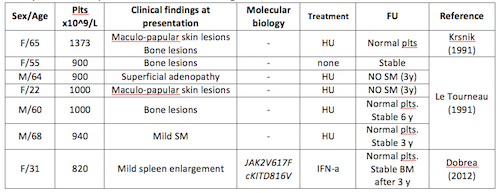
Only seven other patients are described in English literature with ET-SM.
Conclusion
This is the first reported case of ET-SM diagnosed in agreement with the WHO 2016 criteria. Although SM-AHN are considered risk factor for reduced survival, mainly in patients older than 60 years of age, when SM coexists with ET, the less aggressive form among Myeloproliferative Neoplasms (MPN) that does not reduce the patients’ expected survival, prognosis may be doubtful and the absence of mutation in other genes seems to confirm this observation. In the few ET-SM described cases as in our one, HU resulted an efficient and safety treatment.
Session topic: 16. Myeloproliferative neoplasms - Clinical
Keyword(s): Essential Thrombocytemia, Mastocytosis
Abstract: PB2315
Type: Publication Only
Background
Systemic mastocytosis with an associated hematological neoplasm (SM-AHN) is the second most common subtype of SM (estimated frequency 21-44%). In the majority of patients with SM-AHN, a myeloid stem cell malignancy is diagnosed but association of essential thrombocythemia (ET) and SM is anecdotal
Aims
In this work we described a case of Essential Thrmobocythemia associated with Mastocytosis completely diagnosed according to the more recent WHO 2016 criteria and we performed a review of all reported cases in literature about this association.
Methods
We describe a 62 years-old man with thrombocytosis (600-750 x 10^9/L), longstanding hepato-splenomegaly and skin lesions compatible with maculopapular lesions at arms and legs roots (urticaria pigmentosa) treated with phototherapy. The patient had no lymphadenopathy. An abdomen ultrasound revealed fatty liver and splenomegaly (largest dimension 18.7 cm); in addition, lateral X-ray pictures of the thoraco-lumbar spine showed multiple moderate vertebral fractures. Hemoglobin and white cells count were normal; despite a normal ferritin, homozygosity for HFE H63D mutation was detected. We searched for and found JAK2V617F mutation (allele burden 9.3%). The bone marrow (BM) biopsy, showing normal cellularity with normal M:E ratio (3:1), preserved myeloid and erythroid maturation, increased megakaryopoiesis (6-7 megakaryocytes/HPF), large/giant megakaryocytes with hypersegmented nuclei disposed in loose clusters, confirmed the hypothesis of ET. Perivascular and paratrabecular aggregates of spindle-shaped mast cells (MCs) were also present. These cells featured fine metachromatic granules and were intermingled with eosinophils and mature-looking lymphocytes. By immunohistochemistry, MCs were positive for triptase and CD117, with aberrant expression of CD25 and CD2. An increase in bone marrow reticulin fibers (MF grade 2) was present in MC-infiltrated areas. Cytogenetic analysis disclosed a normal male karyotype (46, XY). Elevated serum triptase level (123 ng/mL) and oncogenic KIT D816V mutation definitely established the diagnosis of SM. No mutation in TET2, ASXL1, SRSF2, RUNX1 and CBL genes was found. Treatment with low-dose Aspirin and Hydroxycarbamide (HU) was started and the platelets count rapidly falls to normal values. Two years after diagnosis our patient is alive and in good clinical conditions.
Results
Only seven other patients are described in English literature with ET-SM.
Conclusion
This is the first reported case of ET-SM diagnosed in agreement with the WHO 2016 criteria. Although SM-AHN are considered risk factor for reduced survival, mainly in patients older than 60 years of age, when SM coexists with ET, the less aggressive form among Myeloproliferative Neoplasms (MPN) that does not reduce the patients’ expected survival, prognosis may be doubtful and the absence of mutation in other genes seems to confirm this observation. In the few ET-SM described cases as in our one, HU resulted an efficient and safety treatment.
Session topic: 16. Myeloproliferative neoplasms - Clinical
Keyword(s): Essential Thrombocytemia, Mastocytosis


