
Contributions
Abstract: PB2221
Type: Publication Only
Background
Bone involvement is one of the defining features of symptomatic multiple myeloma (MM). There is little information on changes in bone mineral metabolism that occur with bisphosphonates and anti-myeloma medication.
Aims
Assessment of bone mineral metabolism in MM patients at diagnosis and three months after treatment with antimyeloma drugs and bisphosphonates.
Methods
Newly-diagnosed MM patients were prospectively enrolled from January 2017 to December 2017. Besides standard myeloma work-up (including skeletal survey), baseline evaluation included estimation of serum bone turnover markers [carboxy-terminal cross-linking telopeptide of type I collagen (CTX), aminoterminal propeptide of type 1 procollagen (P1NP), and Osteocalcin (OC)], DEXA scan, and Tc99 bone scintigraphy. Patients were treated as per institutional protocol with antimyeloma drugs and monthly bisphosphonates. Skeletal survey and bone turnover markers were re-assessed after 3 months.
Results
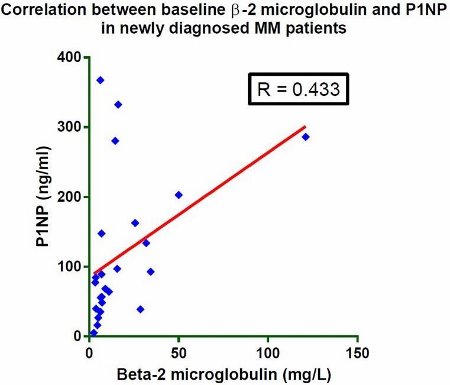
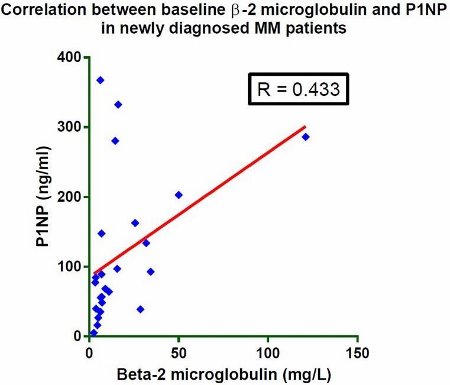
Twenty-four newly-diagnosed MM patients were enrolled. Median age was 55 years (range 35 – 76 years); 79.16% were males. Majority had bone pains (83.3%) and anemia (83.3%); renal failure (45.8%) and hypercalcemia (45.8%) were not uncommon. IgG subtype was most common (52%), followed by IgA (21%) and light chain myeloma (16%). Majority (83.3%) had ISS stage III disease; mean value of β-2 microglobulin was 17.81 (± 25.16) mg/mL. 17 patients (70.83%) had multiple lytic lesions and seven (29.16%) fracture at baseline (pathological 4, traumatic 3). On DEXA scan, 10 patients (41.67%) had osteopenia and three (12.5%) had osteoporosis. Bone scintigraphy revealed meaningful uptake at baseline in 19 patients (79.16%); mainly in axial skeleton. All bone markers [CTX, P1NP, and OC] showed a graded but statistically insignificant correlation with the extent of bone involvement on baseline skeletal survey, P >0.05. Baseline CTX levels in patients with pathological fractures were significantly higher than those without fracture (P = 0.041). Baseline β-2 microglobulin significantly correlated with CTX (r = 0.44) and P1NP (r = 0.43) levels; OC showed no correlation with β-2 microglobulin. After 3 months, significant decline was observed only in CTX levels [0.46 (±0.84) v 1.16 (±1.19), P = 0.001]; minimal upsurge was observed in P1NP and OC levels (P >0.05). Fall in CTX levels among patients receiving VTD [bortezomib, thalidomide plus dexamethasone; n = 5] was significantly greater than those receiving VCD [bortezomib, cyclophosphamide plus dexamethasone; n = 19], P = 0.012. Decline in CTX among patients exclusively treated with zoledronate [n = 17] was significantly larger than those who received initial ibandronate (due to renal failure) followed by zoledronate [n = 7], P = 0.017. After 3 months, overall response rate was 75% [CR 16.7%, VGPR 50%, PR 33.3%].
Conclusion
We observed that bone turnover markers significantly correlated with myeloma disease burden (β-2 microglobulin). Their relationship with the severity of skeletal involvement was graded albeit inconsequential. Bisphosphonates and anti-myeloma medications considerably reduced CTX (bone resorption marker) but had trivial impact on P1NP and OC (bone formation markers). Predominance of ISS stage III patients, small study cohort and mitigation by concomitant unapparent factors (e.g., senile osteoporosis) shall be the possible explanations for these results. Larger prospective studies with longer follow up shall be required to interpret dynamics of bone turnover markers in myeloma.
Session topic: 14. Myeloma and other monoclonal gammopathies - Clinical
Keyword(s): Bisphosphonate, Multiple Myeloma
Abstract: PB2221
Type: Publication Only
Background
Bone involvement is one of the defining features of symptomatic multiple myeloma (MM). There is little information on changes in bone mineral metabolism that occur with bisphosphonates and anti-myeloma medication.
Aims
Assessment of bone mineral metabolism in MM patients at diagnosis and three months after treatment with antimyeloma drugs and bisphosphonates.
Methods
Newly-diagnosed MM patients were prospectively enrolled from January 2017 to December 2017. Besides standard myeloma work-up (including skeletal survey), baseline evaluation included estimation of serum bone turnover markers [carboxy-terminal cross-linking telopeptide of type I collagen (CTX), aminoterminal propeptide of type 1 procollagen (P1NP), and Osteocalcin (OC)], DEXA scan, and Tc99 bone scintigraphy. Patients were treated as per institutional protocol with antimyeloma drugs and monthly bisphosphonates. Skeletal survey and bone turnover markers were re-assessed after 3 months.
Results
Twenty-four newly-diagnosed MM patients were enrolled. Median age was 55 years (range 35 – 76 years); 79.16% were males. Majority had bone pains (83.3%) and anemia (83.3%); renal failure (45.8%) and hypercalcemia (45.8%) were not uncommon. IgG subtype was most common (52%), followed by IgA (21%) and light chain myeloma (16%). Majority (83.3%) had ISS stage III disease; mean value of β-2 microglobulin was 17.81 (± 25.16) mg/mL. 17 patients (70.83%) had multiple lytic lesions and seven (29.16%) fracture at baseline (pathological 4, traumatic 3). On DEXA scan, 10 patients (41.67%) had osteopenia and three (12.5%) had osteoporosis. Bone scintigraphy revealed meaningful uptake at baseline in 19 patients (79.16%); mainly in axial skeleton. All bone markers [CTX, P1NP, and OC] showed a graded but statistically insignificant correlation with the extent of bone involvement on baseline skeletal survey, P >0.05. Baseline CTX levels in patients with pathological fractures were significantly higher than those without fracture (P = 0.041). Baseline β-2 microglobulin significantly correlated with CTX (r = 0.44) and P1NP (r = 0.43) levels; OC showed no correlation with β-2 microglobulin. After 3 months, significant decline was observed only in CTX levels [0.46 (±0.84) v 1.16 (±1.19), P = 0.001]; minimal upsurge was observed in P1NP and OC levels (P >0.05). Fall in CTX levels among patients receiving VTD [bortezomib, thalidomide plus dexamethasone; n = 5] was significantly greater than those receiving VCD [bortezomib, cyclophosphamide plus dexamethasone; n = 19], P = 0.012. Decline in CTX among patients exclusively treated with zoledronate [n = 17] was significantly larger than those who received initial ibandronate (due to renal failure) followed by zoledronate [n = 7], P = 0.017. After 3 months, overall response rate was 75% [CR 16.7%, VGPR 50%, PR 33.3%].
Conclusion
We observed that bone turnover markers significantly correlated with myeloma disease burden (β-2 microglobulin). Their relationship with the severity of skeletal involvement was graded albeit inconsequential. Bisphosphonates and anti-myeloma medications considerably reduced CTX (bone resorption marker) but had trivial impact on P1NP and OC (bone formation markers). Predominance of ISS stage III patients, small study cohort and mitigation by concomitant unapparent factors (e.g., senile osteoporosis) shall be the possible explanations for these results. Larger prospective studies with longer follow up shall be required to interpret dynamics of bone turnover markers in myeloma.
Session topic: 14. Myeloma and other monoclonal gammopathies - Clinical
Keyword(s): Bisphosphonate, Multiple Myeloma


