
Contributions
Abstract: PB2156
Type: Publication Only
Background
Pre-existing pulmonary disease may affect the treatment choices, toxicity and the survival of patients with Multiple Myeloma (MM). However, data on the prognostic value of Pulmonary Function Tests (PFTs) in myeloma patients’ outcome, at the time of initial assessment of newly-diagnosed patients, are scarce.
Aims
To evaluate the incidence and prognostics importance of lung function abnormalities in patients with symptomatic myeloma
Methods
We prospectively performed PFTs in 121 consecutive newly-diagnosed MM patients, before initiation of treatment and we evaluated possible associations of baseline lung function with their outcomes.
Results
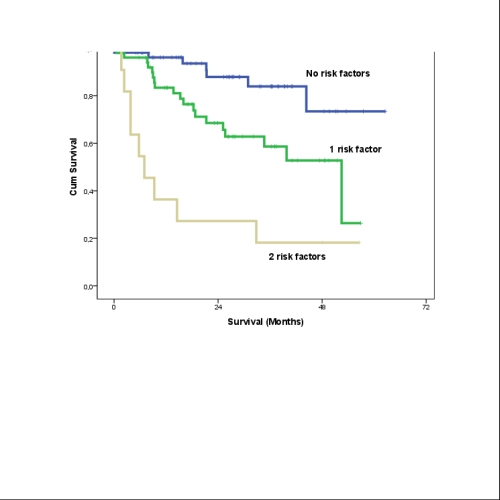
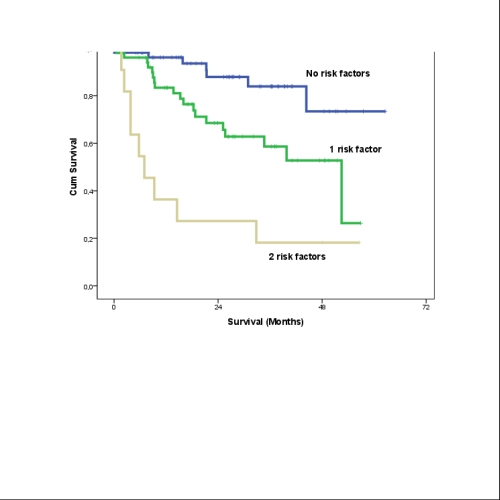
Pulmonary function evaluation with PFTs revealed that 54 patients (44.63%) had either obstructive or restrictive pulmonary function defects, even among patients that did not report a history of lung disease. The survival was significantly worse in patients with obstructive pulmonary defect (median OS: 32.8 months) vs those with restrictive (median OS: 52.5 months) or normal lung function (median not reached, 3-years survival 76%) (p=0.013). In the univariate analysis specific indices of lung function that were associated with survival included Forced Vital Capacity (FVC)(lt)(p=0.012), FVC(%)(p=0.006), Forced Expiratory Volume in 1 sec (FEV1)(lt)(p=0.018), FEV1(%)(p=0.013), Peak Expiratory Flow (PEF)(lt/min)(p=0.008), PEF(%)(p=0.005), carbon monoxide diffusion capacity corrected for hemoglobin (DLCO)(p=0.012), maximal expiratory (Pe)(kPa)(p=0.032) and Pe(%)(p=0.024) and inspiratory pressures (Pi)(kPa)(p=0.023) and Pi(%)(p=0.027). Other baseline factors associated with survival included ISS stage (p=0.008), hypercalcemia (p=0.064), and the presence of high risk cytogenetics (any of t(4;14), t(14;16) or del17p) (p=0.004). Abnormal PFTs were associated with early mortality (<1 year from initiation of therapy). Low PEF was strongly associated with early death (p<0.001); other indices included FVC (p=0.001), FEV1 (p=0.001) and DLCO (p=0.005). Abnormal breathing pattern was also associated with early death, especially obstructive pattern (HR:8, 95%CI 2.1-30, p<0.001) and less restrictive (HR:2.2, 95%CI 0.9-9.7, p=0.068), compared to normal pattern. We identified that PEF <65% of predicted (33 months vs not reached at 3 years, HR:2.8, 95%CI 1.47-5.5, p=0.001) and a DLCO <65% (median OS of 33 months vs not reached, HR:2.54, 95%CI 1.3-5.1, p=0.005) were associated with worse survival. There was a strong association of the two indices (p<0.001): 21% of patients had both, 19% only PEF <65%, 6% only DLCO <65% and 53% none of the two. Multivariate analysis indicated that R-ISS-3 and the presence of either or both PEF(%)<65% and DLCO<65% of predicted were the strongest prognostic factors for survival. Thus, we formulated a prognostic score encompassing myeloma-related and myeloma-independent factors that discriminates 3 groups with different survival: 3 year survival was 85% and 59% for patients with none or either of the risk factors and 18% (median survival of 7 months) if they had both (p<0.001) (see figure). Importantly, the prognostic significance of this score was independent of the age of the patients.
Conclusion
We conclude that PEF and DLCO could be useful in the initial assessment of newly-diagnosed MM patients as significant predictors of survival. Respiratory screening should be included in the routine initial evaluation of myeloma patients, despite the presence or absence of respiratory symptoms or abnormal clinical respiratory examination.
Session topic: 14. Myeloma and other monoclonal gammopathies - Clinical
Keyword(s): Lung, Myeloma, Prognostic factor
Abstract: PB2156
Type: Publication Only
Background
Pre-existing pulmonary disease may affect the treatment choices, toxicity and the survival of patients with Multiple Myeloma (MM). However, data on the prognostic value of Pulmonary Function Tests (PFTs) in myeloma patients’ outcome, at the time of initial assessment of newly-diagnosed patients, are scarce.
Aims
To evaluate the incidence and prognostics importance of lung function abnormalities in patients with symptomatic myeloma
Methods
We prospectively performed PFTs in 121 consecutive newly-diagnosed MM patients, before initiation of treatment and we evaluated possible associations of baseline lung function with their outcomes.
Results
Pulmonary function evaluation with PFTs revealed that 54 patients (44.63%) had either obstructive or restrictive pulmonary function defects, even among patients that did not report a history of lung disease. The survival was significantly worse in patients with obstructive pulmonary defect (median OS: 32.8 months) vs those with restrictive (median OS: 52.5 months) or normal lung function (median not reached, 3-years survival 76%) (p=0.013). In the univariate analysis specific indices of lung function that were associated with survival included Forced Vital Capacity (FVC)(lt)(p=0.012), FVC(%)(p=0.006), Forced Expiratory Volume in 1 sec (FEV1)(lt)(p=0.018), FEV1(%)(p=0.013), Peak Expiratory Flow (PEF)(lt/min)(p=0.008), PEF(%)(p=0.005), carbon monoxide diffusion capacity corrected for hemoglobin (DLCO)(p=0.012), maximal expiratory (Pe)(kPa)(p=0.032) and Pe(%)(p=0.024) and inspiratory pressures (Pi)(kPa)(p=0.023) and Pi(%)(p=0.027). Other baseline factors associated with survival included ISS stage (p=0.008), hypercalcemia (p=0.064), and the presence of high risk cytogenetics (any of t(4;14), t(14;16) or del17p) (p=0.004). Abnormal PFTs were associated with early mortality (<1 year from initiation of therapy). Low PEF was strongly associated with early death (p<0.001); other indices included FVC (p=0.001), FEV1 (p=0.001) and DLCO (p=0.005). Abnormal breathing pattern was also associated with early death, especially obstructive pattern (HR:8, 95%CI 2.1-30, p<0.001) and less restrictive (HR:2.2, 95%CI 0.9-9.7, p=0.068), compared to normal pattern. We identified that PEF <65% of predicted (33 months vs not reached at 3 years, HR:2.8, 95%CI 1.47-5.5, p=0.001) and a DLCO <65% (median OS of 33 months vs not reached, HR:2.54, 95%CI 1.3-5.1, p=0.005) were associated with worse survival. There was a strong association of the two indices (p<0.001): 21% of patients had both, 19% only PEF <65%, 6% only DLCO <65% and 53% none of the two. Multivariate analysis indicated that R-ISS-3 and the presence of either or both PEF(%)<65% and DLCO<65% of predicted were the strongest prognostic factors for survival. Thus, we formulated a prognostic score encompassing myeloma-related and myeloma-independent factors that discriminates 3 groups with different survival: 3 year survival was 85% and 59% for patients with none or either of the risk factors and 18% (median survival of 7 months) if they had both (p<0.001) (see figure). Importantly, the prognostic significance of this score was independent of the age of the patients.
Conclusion
We conclude that PEF and DLCO could be useful in the initial assessment of newly-diagnosed MM patients as significant predictors of survival. Respiratory screening should be included in the routine initial evaluation of myeloma patients, despite the presence or absence of respiratory symptoms or abnormal clinical respiratory examination.
Session topic: 14. Myeloma and other monoclonal gammopathies - Clinical
Keyword(s): Lung, Myeloma, Prognostic factor


