
Contributions
Abstract: PB2216
Type: Publication Only
Background
Solitary plasmacytoma (SP) is a plasma cell dyscrasia that presents as a mass lesion consists of plasma cells that produces monoclonal immunoglobulins without any systemic involvement. SP accounts for approximately 5% of all plasma cell dyscrasias and mostly occurs in osseous tissue, however one third of patients have extramedullary plasmacytoma.
Aims
In this paper, we analyzed our patients and aimed to reveal patient characteristics and outcomes.
Methods
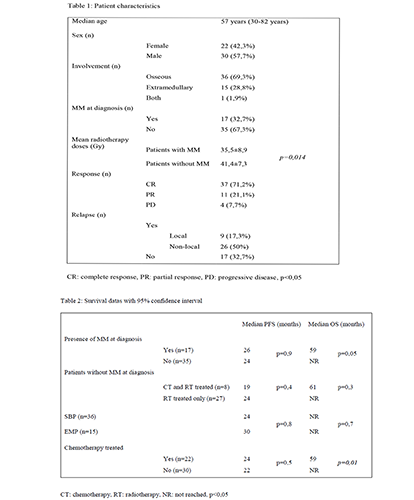
A total of 52 patients who were referred to our clinics of hematology and radiation oncology with the diagnosis of SP from January 2006 to March 2017, were evaluated retrospectively. Age, sex, treatment procedures, radiotherapy doses, involved tissue datas, relapse and response status, death times were recorded from hospital registries.
Results
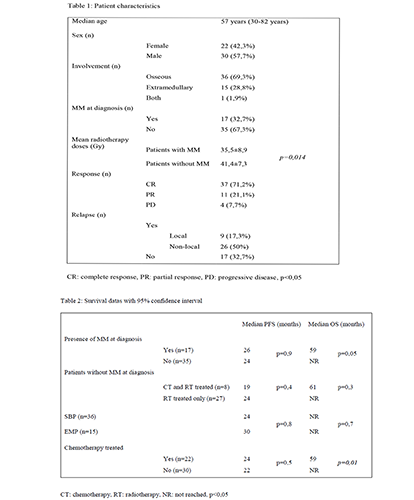
Median age at the diagnosis was 57 years (30-82 years), 57,7% of them (n=30) were male. Seventeen patients were diagnosed as concurrent multiple myeloma (MM) and 15 of those treated with radiotherapy and chemotherapy both. Patients without MM at the diagnosis (n=35) were irradiated and followed periodically after completion of radiotherapy, 8 of those were treated with chemotherapy adjacent to radiotherapy due to widespread disease. Solitary bone plasmacytoma (SBP) was the most common diagnosis with a rate of 69,2% (n=36), one patient was diagnosed with SBP and extramedullary plasmacytoma (EMP) at the same time. Patients those whom had concurrent MM was irradiated palliatively with a dose of 20 to 45 Gray (Gy), curative radiotherapy was performed to all other patients at a dose of 45 to 54 Gy. Median duration of follow-up for patients was 45 months (0-144 months). Local recurrence defined as relapse from the affected site at the diagnosis was detected in 9 patients (17,3%), all relapsing patients (67,3%, n=35) were received mean 38,2±9,0 Gy dose of irradiation while patients with no recurrence were treated with mean 42,2±5,8 Gy dose of irradiation during diagnosis. Local recurrence was not related with the dose of radiotherapy (p=0,5). Patients responded well to all therapies, partial and complete response were achieved in 92,3% of patients (n=48). During follow-up MM was diagnosed in 7 of all 35 patients without MM at the time of diagnosis, five of them had SBP. Median progression time to MM for those patients was 29 months (14-104 months). Median overall survival (OS) was not achieved, progression free survival (PFS) was median 26 months. The presence of MM at the diagnosis was not a risk factor for progressive disease (p=0,9). Median OS for patients with MM at the diagnosis was 59 months and was not reached in patients without MM. There were no significant PFS and OS differences between SBP and EMP groups (p=0,8, p=0,7, respectively). The outcomes of patients without concurrent MM treated with chemo-radiotherapy and treated with radiotherapy alone were not different also (Table 2).
Conclusion
This registry-based study represents our experience on SP and provides the data showing that radiotherapy as a single regimen results in good outcomes. Due to limited number of patient, it is difficult to hypothesize that radiotherapy is the golden standard, but radiotherapy alone to involved area seems to be adequate and safe treatment option. Our findings is consistent with literature, however there is no prospective or large patient group of retrospective analysis in the literature.
Session topic: 14. Myeloma and other monoclonal gammopathies - Clinical
Keyword(s): chemotherapy, Myeloma, Plasma cells, Radiotherapy
Abstract: PB2216
Type: Publication Only
Background
Solitary plasmacytoma (SP) is a plasma cell dyscrasia that presents as a mass lesion consists of plasma cells that produces monoclonal immunoglobulins without any systemic involvement. SP accounts for approximately 5% of all plasma cell dyscrasias and mostly occurs in osseous tissue, however one third of patients have extramedullary plasmacytoma.
Aims
In this paper, we analyzed our patients and aimed to reveal patient characteristics and outcomes.
Methods
A total of 52 patients who were referred to our clinics of hematology and radiation oncology with the diagnosis of SP from January 2006 to March 2017, were evaluated retrospectively. Age, sex, treatment procedures, radiotherapy doses, involved tissue datas, relapse and response status, death times were recorded from hospital registries.
Results
Median age at the diagnosis was 57 years (30-82 years), 57,7% of them (n=30) were male. Seventeen patients were diagnosed as concurrent multiple myeloma (MM) and 15 of those treated with radiotherapy and chemotherapy both. Patients without MM at the diagnosis (n=35) were irradiated and followed periodically after completion of radiotherapy, 8 of those were treated with chemotherapy adjacent to radiotherapy due to widespread disease. Solitary bone plasmacytoma (SBP) was the most common diagnosis with a rate of 69,2% (n=36), one patient was diagnosed with SBP and extramedullary plasmacytoma (EMP) at the same time. Patients those whom had concurrent MM was irradiated palliatively with a dose of 20 to 45 Gray (Gy), curative radiotherapy was performed to all other patients at a dose of 45 to 54 Gy. Median duration of follow-up for patients was 45 months (0-144 months). Local recurrence defined as relapse from the affected site at the diagnosis was detected in 9 patients (17,3%), all relapsing patients (67,3%, n=35) were received mean 38,2±9,0 Gy dose of irradiation while patients with no recurrence were treated with mean 42,2±5,8 Gy dose of irradiation during diagnosis. Local recurrence was not related with the dose of radiotherapy (p=0,5). Patients responded well to all therapies, partial and complete response were achieved in 92,3% of patients (n=48). During follow-up MM was diagnosed in 7 of all 35 patients without MM at the time of diagnosis, five of them had SBP. Median progression time to MM for those patients was 29 months (14-104 months). Median overall survival (OS) was not achieved, progression free survival (PFS) was median 26 months. The presence of MM at the diagnosis was not a risk factor for progressive disease (p=0,9). Median OS for patients with MM at the diagnosis was 59 months and was not reached in patients without MM. There were no significant PFS and OS differences between SBP and EMP groups (p=0,8, p=0,7, respectively). The outcomes of patients without concurrent MM treated with chemo-radiotherapy and treated with radiotherapy alone were not different also (Table 2).
Conclusion
This registry-based study represents our experience on SP and provides the data showing that radiotherapy as a single regimen results in good outcomes. Due to limited number of patient, it is difficult to hypothesize that radiotherapy is the golden standard, but radiotherapy alone to involved area seems to be adequate and safe treatment option. Our findings is consistent with literature, however there is no prospective or large patient group of retrospective analysis in the literature.
Session topic: 14. Myeloma and other monoclonal gammopathies - Clinical
Keyword(s): chemotherapy, Myeloma, Plasma cells, Radiotherapy


