
Contributions
Abstract: PB2180
Type: Publication Only
Background
Multiple myeloma (MM) is a clonal plasma cell malignancy that is increasing in prevalence as the population ages and the survival improves. Infection is a leading cause of morbidity and mortality, contributing to nearly 50% of early deaths (Augustson et al, 2005). Infection risk is increased due to patient-, disease- and treatment-related factors. New treatment options in the last decades have improve survival in MM patients but their effect on the risk of infections remains to be established yet.
Aims
To describe retrospectively the development of infections requiring hospitalization in 91 MM patients diagnosed in our institution between 2008 and 2017.
Methods
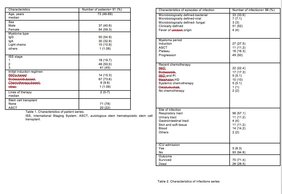
Median age 73 years (46-89), 54 females. There were 51 patients with 1 or 2 infections and 9 patients with > 3 infections. 31 patients had no infection. Characteristics of the studied patients are detailed in Table 1.
Results
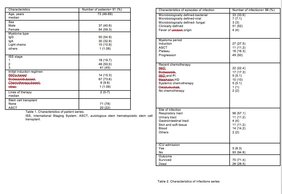
98 episodes of infection were identified. Of these, 43 (43.8%) were microbiologically identified, 51 (52%) clinically defined and 4 (4%) were fever of unknown origin. Of the 43 microbiologically defined infections, 77% (33) were bacterial, 7% (3) fungal and 16.2% (7) viral. Of the 33 bacterial infections, 18 (54.5%) were caused by gram negative and 15 (45.4%) gram positive microorganisms. Escherichia Coli was the most frequently isolated organism (21%). Vaccine-preventable encapsulated bacteria Str.pneumoniae was isolated in 18% of all bacterial infections. The 7 viral infections were due to influenza virus (57%), respiratory syncytial virus (28%) and herpes simplex reactivation (14%).There were 3 fungal infections: 2 candidemias and 1 Pneumocystis Jiroveci pneumonia. Respiratory tract (57,1%) and blood (14.2%) were the most common sites of infection. Bacterial infections occurred more frequently in relapse phases (84%), during neutropenia (53%) or in hypogammaglobulinemic patients (62%).All the patients with viral-infections had previous PIs (Proteosome Inhibitors) based therapies. All the patients with fungal-infections had previous IMiDs (Immunomodulatory drugs) therapies and were receiving HD (high dose) steroids.Infections occurred more frequently at disease progression (50%) and during induction (27.5%) and the majority of patients were older than 65 (74%). 11/16 infections occurring during plateau were of low severity and had good outcome.Most recent therapies administered before infection development were IMiDs (22,4%) and Bortezomib (17.3%). Admission to the intensive care unit (ICU) was required in 8.3% infection episodes. 28 infections resulted in death (28.5%): 22/28 occurring during disease progression, 2/28 during induction (1 patient with herpetic encephalitis and 1 multiorganic failure MOF), 1 in ASCT and 3 deaths during plateau (1 heart failure in VGPR, 1 MOF after prolonged hospitalization for toxicity in PR, 1 pneumococcal pneumonia in CR). Overall Survival (OS) was 63 months. More details of infections are shown in table 2.
Conclusion
Our study identifies a high risk patient group for infections: older age, late disease, advanced ISS, multiple treatments, HD corticoids treatments. Infections represent a significant-comorbidity factor especially during induction and in refractory/relapsed-patients, with 28.5% infection related mortality in our population. Immunoglobulin replacement therapy, vaccination for encapsulated bacteria or antibiotic-prophylaxis may have a role in older patients with high ISS stage. Trials are needed to target new approaches for prevention, early detection and treatment of infection in MM patients.
Session topic: 14. Myeloma and other monoclonal gammopathies - Clinical
Keyword(s): Imids, Infection, Prevention, Treatment
Abstract: PB2180
Type: Publication Only
Background
Multiple myeloma (MM) is a clonal plasma cell malignancy that is increasing in prevalence as the population ages and the survival improves. Infection is a leading cause of morbidity and mortality, contributing to nearly 50% of early deaths (Augustson et al, 2005). Infection risk is increased due to patient-, disease- and treatment-related factors. New treatment options in the last decades have improve survival in MM patients but their effect on the risk of infections remains to be established yet.
Aims
To describe retrospectively the development of infections requiring hospitalization in 91 MM patients diagnosed in our institution between 2008 and 2017.
Methods
Median age 73 years (46-89), 54 females. There were 51 patients with 1 or 2 infections and 9 patients with > 3 infections. 31 patients had no infection. Characteristics of the studied patients are detailed in Table 1.
Results
98 episodes of infection were identified. Of these, 43 (43.8%) were microbiologically identified, 51 (52%) clinically defined and 4 (4%) were fever of unknown origin. Of the 43 microbiologically defined infections, 77% (33) were bacterial, 7% (3) fungal and 16.2% (7) viral. Of the 33 bacterial infections, 18 (54.5%) were caused by gram negative and 15 (45.4%) gram positive microorganisms. Escherichia Coli was the most frequently isolated organism (21%). Vaccine-preventable encapsulated bacteria Str.pneumoniae was isolated in 18% of all bacterial infections. The 7 viral infections were due to influenza virus (57%), respiratory syncytial virus (28%) and herpes simplex reactivation (14%).There were 3 fungal infections: 2 candidemias and 1 Pneumocystis Jiroveci pneumonia. Respiratory tract (57,1%) and blood (14.2%) were the most common sites of infection. Bacterial infections occurred more frequently in relapse phases (84%), during neutropenia (53%) or in hypogammaglobulinemic patients (62%).All the patients with viral-infections had previous PIs (Proteosome Inhibitors) based therapies. All the patients with fungal-infections had previous IMiDs (Immunomodulatory drugs) therapies and were receiving HD (high dose) steroids.Infections occurred more frequently at disease progression (50%) and during induction (27.5%) and the majority of patients were older than 65 (74%). 11/16 infections occurring during plateau were of low severity and had good outcome.Most recent therapies administered before infection development were IMiDs (22,4%) and Bortezomib (17.3%). Admission to the intensive care unit (ICU) was required in 8.3% infection episodes. 28 infections resulted in death (28.5%): 22/28 occurring during disease progression, 2/28 during induction (1 patient with herpetic encephalitis and 1 multiorganic failure MOF), 1 in ASCT and 3 deaths during plateau (1 heart failure in VGPR, 1 MOF after prolonged hospitalization for toxicity in PR, 1 pneumococcal pneumonia in CR). Overall Survival (OS) was 63 months. More details of infections are shown in table 2.
Conclusion
Our study identifies a high risk patient group for infections: older age, late disease, advanced ISS, multiple treatments, HD corticoids treatments. Infections represent a significant-comorbidity factor especially during induction and in refractory/relapsed-patients, with 28.5% infection related mortality in our population. Immunoglobulin replacement therapy, vaccination for encapsulated bacteria or antibiotic-prophylaxis may have a role in older patients with high ISS stage. Trials are needed to target new approaches for prevention, early detection and treatment of infection in MM patients.
Session topic: 14. Myeloma and other monoclonal gammopathies - Clinical
Keyword(s): Imids, Infection, Prevention, Treatment


