
Contributions
Abstract: PB2141
Type: Publication Only
Background
Renal impairment (RI) is a common complication of multiple myeloma (MM), which significantly affects not only treatment efficacy but also patient mortality. The conventional parameters defining RI in MM (the level of serum creatinine (Cr) > 2.00 mg/dl or Ccr < 40 ml/min) are not sensitive, resulting in the delay of diagnosis and treatment of RI. Recently, it is reported that monoclonal gammopathy of renal significance (MGRS), which represents all renal disorders caused by a monoclonal immunoglobulin secreted by a B-cell or plasma cell clone, is associated with high morbidity. Therefore, sensitive reliable parameters for early diagnosis of RI in MM are required. Activin A, a multifunctional cytokine belonging to the TGF-β superfamily, has been reported to be involved in kidney development, tubular repair after injury and fibrotic process of the kidney. However, it is unclear whether activin A plays a role in renal damages in MM.
Aims
To clarify the involvement of activin A in renal damages in MM, we examined whether activin A can be detectable in the urine from patients with newly diagnosed MM (NDMM), asymptomatic (smoldering) (SMM), and MGUS including MGRS.
Methods
We investigated the data of patients with NDMM (n=41), SMM (n=10), and MGUS (n=28) diagnosed in our department between October 2012 and September 2017. Along with common blood and urine chemistry determinations, serum and urinary activin A were measured by ELISA. In some cases, renal histological evaluation was performed using renal biopsy samples. This study was approved by the local institutional review board, and written informed consent was obtained from all patients.
Results
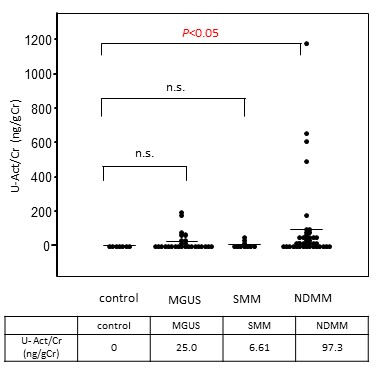
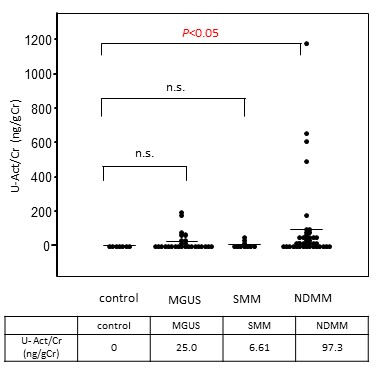
Urinary activin A, which was undetectable in healthy controls (HC), significantly increased in NDMM (97.3 ± 36.0 ng/gCr, p<0.05 vs. HC), but not in MGUS (25.0 ± 9.4 ng/gCr) and SMM (6.61 ± 3.9 ng/gCr). There were no significant differences in serum activin A level among these subgroups. Urinary activin A level was significantly reduced after initial treatment in NDMM (73.9 vs 12.0 ng/gCr, p<0.01). Improvement rate of urinary activin A from baseline after treatment was much higher than that of serum Cr or eGFR (84%, 30%, 12%, respectively). There was a significant correlation of urinary activin A with urinary protein level (p<0.001), but not with eGFR, serum Cr, and N-acetyl-glucosaminidase. Interestingly, there was no significant correlation between serum and urinary activin A level. Immunohistochemical analysis revealed that activin A, which was absent in normal kidney, was present at the tubulointerstitial area of the kidneys from patients with MGRS.
Conclusion
These data suggest that urinary activin A is a novel urinary biomarker detecting renal damages in MM. Measurement of urinary activin A might be an useful tool to perform early diagnosis of RI or to predict the severity of renal damages in MM.
Session topic: 13. Myeloma and other monoclonal gammopathies – Biology & Translational Research
Keyword(s): MGUS, Multiple Myeloma, Renal impairment
Abstract: PB2141
Type: Publication Only
Background
Renal impairment (RI) is a common complication of multiple myeloma (MM), which significantly affects not only treatment efficacy but also patient mortality. The conventional parameters defining RI in MM (the level of serum creatinine (Cr) > 2.00 mg/dl or Ccr < 40 ml/min) are not sensitive, resulting in the delay of diagnosis and treatment of RI. Recently, it is reported that monoclonal gammopathy of renal significance (MGRS), which represents all renal disorders caused by a monoclonal immunoglobulin secreted by a B-cell or plasma cell clone, is associated with high morbidity. Therefore, sensitive reliable parameters for early diagnosis of RI in MM are required. Activin A, a multifunctional cytokine belonging to the TGF-β superfamily, has been reported to be involved in kidney development, tubular repair after injury and fibrotic process of the kidney. However, it is unclear whether activin A plays a role in renal damages in MM.
Aims
To clarify the involvement of activin A in renal damages in MM, we examined whether activin A can be detectable in the urine from patients with newly diagnosed MM (NDMM), asymptomatic (smoldering) (SMM), and MGUS including MGRS.
Methods
We investigated the data of patients with NDMM (n=41), SMM (n=10), and MGUS (n=28) diagnosed in our department between October 2012 and September 2017. Along with common blood and urine chemistry determinations, serum and urinary activin A were measured by ELISA. In some cases, renal histological evaluation was performed using renal biopsy samples. This study was approved by the local institutional review board, and written informed consent was obtained from all patients.
Results
Urinary activin A, which was undetectable in healthy controls (HC), significantly increased in NDMM (97.3 ± 36.0 ng/gCr, p<0.05 vs. HC), but not in MGUS (25.0 ± 9.4 ng/gCr) and SMM (6.61 ± 3.9 ng/gCr). There were no significant differences in serum activin A level among these subgroups. Urinary activin A level was significantly reduced after initial treatment in NDMM (73.9 vs 12.0 ng/gCr, p<0.01). Improvement rate of urinary activin A from baseline after treatment was much higher than that of serum Cr or eGFR (84%, 30%, 12%, respectively). There was a significant correlation of urinary activin A with urinary protein level (p<0.001), but not with eGFR, serum Cr, and N-acetyl-glucosaminidase. Interestingly, there was no significant correlation between serum and urinary activin A level. Immunohistochemical analysis revealed that activin A, which was absent in normal kidney, was present at the tubulointerstitial area of the kidneys from patients with MGRS.
Conclusion
These data suggest that urinary activin A is a novel urinary biomarker detecting renal damages in MM. Measurement of urinary activin A might be an useful tool to perform early diagnosis of RI or to predict the severity of renal damages in MM.
Session topic: 13. Myeloma and other monoclonal gammopathies – Biology & Translational Research
Keyword(s): MGUS, Multiple Myeloma, Renal impairment


