
Contributions
Abstract: PB1824
Type: Publication Only
Background
Clonal expansion or its clinical impact after immunosuppressive therapy (IST) was not fully elucidated in patients with paroxysmal nocturnal hemoglobinuria (PNH) in the context of aplastic anemia (AA) (AA/PNH).
Aims
This study aimed to identify the dynamics of PNH clone and proportion of hemolytic manifestations according to baseline clone size during the course of AA/PNH after IST.
Methods
A cohort of 63 patients who received IST at the time of diagnosis of AA/PNH was enrolled in this study. Hemolytic AA/PNH was defined as AA/PNH with elevated lactate dehydrogenase (LDH) ≥ 1.5 times the upper limit of normal (ULN). Data of each PNH clone were collected at diagnosis, 6, 12, 24 months after diagnosis of AA/PNH. PNH clone of granulocyte was measured by high-sensitivity flow cytometry (FC). The sensitivity limit of FC was 0.01% of granulocyte population. We divided patients into two groups according to granulocyte clone size at the time of diagnosis for AA/PNH: group-A (n=17) consisted of patients who showed PNH clone size ≤1%, and group-B (n=46) patients who had PNH clone size >1%.
Results
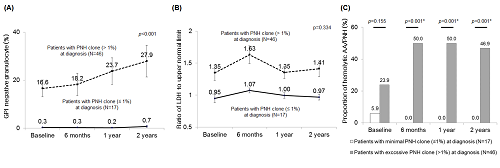
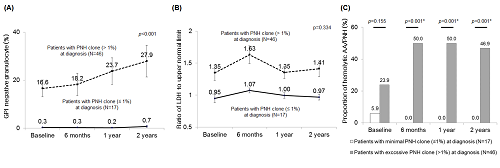
The median age of patients was 44 years (range, 18-79) and 12 patients (19.0%) had hemolytic AA/PNH at diagnosis of AA/PNH. During median follow-up periods of 36.0 months (5.8-90.6) from diagnosis of AA/PNH, overall response rate (ORR) of IST was 82.5% without significant intergroup difference between group-A and B (88.2% vs. 80.4%, p=0.712). The median clone size and LDH value were 2.5% (range, 0.1-85.7) and 1.07 (range, 0.50-4.36) x ULN, respectively. Twenty-five patients (39.7%) developed hemolytic AA/PNH during the clinical course. Compared to dynamics of group-A, those of group-B showed significant upward trend of clone size over time (p<0.001) (Fig A). After 2-years from diagnosis, average PNH close size of group B was significantly increased from the baseline (16.6% at diagnosis to 27.9% at 2 years, p=0.024), whereas that of group A was not changed (0.3% at diagnosis to 0.7% at 2-years, p=0.932). There were no significant difference of median LDH value between baseline and 2-year in both groups (0.95x ULN to 0.97x ULN in group A, p=0.600, whereas 1.35x ULN to 1.41x ULN in group B, p=0.063) (Fig B). However, despite similar frequencies of hemolytic AA/PNH at baseline between group-A and B (5.9% in group-A vs. 23.9% in group-B, p=0.155), the proportions of hemolytic AA/PNH in group-B were significantly higher at 2-year compared to those of group-A (46.9% vs. 0.0%, p<0.001) (Fig C).
Conclusion
Current study demonstrate that there were significant differences in the dynamics of the PNH clone and its hemolytic manifestations according to 1% of baseline PNH clone size as cut-off in patients with AA/PNH after IST. Although ORR of IST was similar between two groups, it is suggested that the regular monitoring of PNH clone and LDH value in AA/PNH should be performed in patients with clone size >1% at baseline to identify the clonal expansion and hemolytic manifestations earlier after IST.
Session topic: 12. Bone marrow failure syndromes incl. PNH - Clinical
Keyword(s): Aplastic anemia, Clonal expansion, flow cytometry, Paroxysmal nocturnal hemoglobinuria (PNH)
Abstract: PB1824
Type: Publication Only
Background
Clonal expansion or its clinical impact after immunosuppressive therapy (IST) was not fully elucidated in patients with paroxysmal nocturnal hemoglobinuria (PNH) in the context of aplastic anemia (AA) (AA/PNH).
Aims
This study aimed to identify the dynamics of PNH clone and proportion of hemolytic manifestations according to baseline clone size during the course of AA/PNH after IST.
Methods
A cohort of 63 patients who received IST at the time of diagnosis of AA/PNH was enrolled in this study. Hemolytic AA/PNH was defined as AA/PNH with elevated lactate dehydrogenase (LDH) ≥ 1.5 times the upper limit of normal (ULN). Data of each PNH clone were collected at diagnosis, 6, 12, 24 months after diagnosis of AA/PNH. PNH clone of granulocyte was measured by high-sensitivity flow cytometry (FC). The sensitivity limit of FC was 0.01% of granulocyte population. We divided patients into two groups according to granulocyte clone size at the time of diagnosis for AA/PNH: group-A (n=17) consisted of patients who showed PNH clone size ≤1%, and group-B (n=46) patients who had PNH clone size >1%.
Results
The median age of patients was 44 years (range, 18-79) and 12 patients (19.0%) had hemolytic AA/PNH at diagnosis of AA/PNH. During median follow-up periods of 36.0 months (5.8-90.6) from diagnosis of AA/PNH, overall response rate (ORR) of IST was 82.5% without significant intergroup difference between group-A and B (88.2% vs. 80.4%, p=0.712). The median clone size and LDH value were 2.5% (range, 0.1-85.7) and 1.07 (range, 0.50-4.36) x ULN, respectively. Twenty-five patients (39.7%) developed hemolytic AA/PNH during the clinical course. Compared to dynamics of group-A, those of group-B showed significant upward trend of clone size over time (p<0.001) (Fig A). After 2-years from diagnosis, average PNH close size of group B was significantly increased from the baseline (16.6% at diagnosis to 27.9% at 2 years, p=0.024), whereas that of group A was not changed (0.3% at diagnosis to 0.7% at 2-years, p=0.932). There were no significant difference of median LDH value between baseline and 2-year in both groups (0.95x ULN to 0.97x ULN in group A, p=0.600, whereas 1.35x ULN to 1.41x ULN in group B, p=0.063) (Fig B). However, despite similar frequencies of hemolytic AA/PNH at baseline between group-A and B (5.9% in group-A vs. 23.9% in group-B, p=0.155), the proportions of hemolytic AA/PNH in group-B were significantly higher at 2-year compared to those of group-A (46.9% vs. 0.0%, p<0.001) (Fig C).
Conclusion
Current study demonstrate that there were significant differences in the dynamics of the PNH clone and its hemolytic manifestations according to 1% of baseline PNH clone size as cut-off in patients with AA/PNH after IST. Although ORR of IST was similar between two groups, it is suggested that the regular monitoring of PNH clone and LDH value in AA/PNH should be performed in patients with clone size >1% at baseline to identify the clonal expansion and hemolytic manifestations earlier after IST.
Session topic: 12. Bone marrow failure syndromes incl. PNH - Clinical
Keyword(s): Aplastic anemia, Clonal expansion, flow cytometry, Paroxysmal nocturnal hemoglobinuria (PNH)


