
Contributions
Abstract: PB2095
Type: Publication Only
Background
Diabetes mellitus (DM) is a common co-morbidity in patients with myelodysplastic syndromes (MDS). In the general population, DM is associated with a shorter life expectancy, greater risk for infection, and anemia even in the absence of severe renal disease. It would be reasonable to assume that these issues would have a considerable impact on the management and outcomes of patients with MDS and DM.
Aims
We aimed to determine differences in the clinical chracteristics and disease course of diabetic vs. non-diabetic MDS patients.
Methods
We retrospectively analyzed the characteristics and survival of MDS patients from four medical centers in Israel. We compared disease parameters at presentation, co-morbidities and overall survival between diabetic MDS patients and non-diabetic MDS patients.
Results
We reviewed records of 700 patients diagnosed with MDS between 2004 and 2016. Of these, 185 MDS patients (26.4%) had DM prior to MDS. The median age (75 vs. 76.5, p=0.322) and gender distribution (43.3% vs. 40.5% females, p=0.581) were similar for MDS patients with and without DM, respectively. Diabetic patients had a higher median body mass index (27.7 vs. 26.7, p=0.02).
MDS patients with DM had more co-morbidities than non-diabetic patients: cardiovascular disease (32.9% vs. 22.6%, p=0.018), chronic kidney disease (37.8% vs. 19.2% p<0.001), and hypertension (89.6% vs. 67.7% p<0.001). COPD and history of previous chemotherapy were not significantly different between the two groups.
Among patients with sufficient data to assign an IPSS-R risk category (n=259) diabetic patients had a trend towards lower risk disease (IPSS-R very low/low in 76% of diabetics vs. 66% non-diabetic, p=0.09).
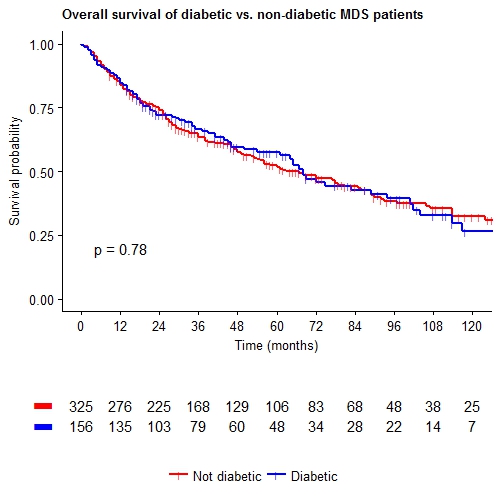
Survival data were available for 481 patients. Median follow-up time was 74 months (95% CI 64-87 months). We observed no significant difference in overall survival curves or median overall survival between diabetic and non-diabetic MDS patients (Figure 1) (median OS 67.7 months 95% CI 57-78.3 months vs. 62.9 months 95% CI 48-77.8 months, p=0.778).
Conclusion
MDS patients with DM have more co-morbidities than MDS patients who are non-diabetic. In contrast to expectations, in our series, diabetic and non-diabetic patients with MDS had similar overall survival. Additional studies are needed to confirm this finding, and to elucidate whether this is due to specific biological differences between diabetic and non-diabetic MDS patients or whether this is due to closer medical follow-up of diabetic patients, leading to diagnosis of MDS in earlier stages.
Session topic: 10. Myelodysplastic syndromes – Clinical
Keyword(s): Clinical data, Comorbidities, Myelodysplasia, Survival
Abstract: PB2095
Type: Publication Only
Background
Diabetes mellitus (DM) is a common co-morbidity in patients with myelodysplastic syndromes (MDS). In the general population, DM is associated with a shorter life expectancy, greater risk for infection, and anemia even in the absence of severe renal disease. It would be reasonable to assume that these issues would have a considerable impact on the management and outcomes of patients with MDS and DM.
Aims
We aimed to determine differences in the clinical chracteristics and disease course of diabetic vs. non-diabetic MDS patients.
Methods
We retrospectively analyzed the characteristics and survival of MDS patients from four medical centers in Israel. We compared disease parameters at presentation, co-morbidities and overall survival between diabetic MDS patients and non-diabetic MDS patients.
Results
We reviewed records of 700 patients diagnosed with MDS between 2004 and 2016. Of these, 185 MDS patients (26.4%) had DM prior to MDS. The median age (75 vs. 76.5, p=0.322) and gender distribution (43.3% vs. 40.5% females, p=0.581) were similar for MDS patients with and without DM, respectively. Diabetic patients had a higher median body mass index (27.7 vs. 26.7, p=0.02).
MDS patients with DM had more co-morbidities than non-diabetic patients: cardiovascular disease (32.9% vs. 22.6%, p=0.018), chronic kidney disease (37.8% vs. 19.2% p<0.001), and hypertension (89.6% vs. 67.7% p<0.001). COPD and history of previous chemotherapy were not significantly different between the two groups.
Among patients with sufficient data to assign an IPSS-R risk category (n=259) diabetic patients had a trend towards lower risk disease (IPSS-R very low/low in 76% of diabetics vs. 66% non-diabetic, p=0.09).
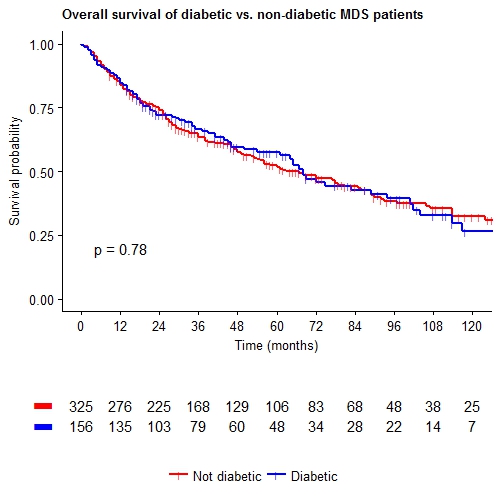
Survival data were available for 481 patients. Median follow-up time was 74 months (95% CI 64-87 months). We observed no significant difference in overall survival curves or median overall survival between diabetic and non-diabetic MDS patients (Figure 1) (median OS 67.7 months 95% CI 57-78.3 months vs. 62.9 months 95% CI 48-77.8 months, p=0.778).
Conclusion
MDS patients with DM have more co-morbidities than MDS patients who are non-diabetic. In contrast to expectations, in our series, diabetic and non-diabetic patients with MDS had similar overall survival. Additional studies are needed to confirm this finding, and to elucidate whether this is due to specific biological differences between diabetic and non-diabetic MDS patients or whether this is due to closer medical follow-up of diabetic patients, leading to diagnosis of MDS in earlier stages.
Session topic: 10. Myelodysplastic syndromes – Clinical
Keyword(s): Clinical data, Comorbidities, Myelodysplasia, Survival


