
Contributions
Abstract: PB2096
Type: Publication Only
Background
Multiple autoimmune conditions have been described in the context of chronic myelomonocytic leukemia (CMML), but it is not clear if they could have an impact on clinical evolution.
Aims
We describe the subgroup of CMML related to autoimmune diseases (AD) and the main clinical features, compared to the patients who have other types of CMML.
Methods
We have studied 38 patients over 14 years (2003-2016), and compared the subgroup with autoimmune versus non-autoimmune disorders, in order to establish differences in some clinical parameters and the free progression survival (PFS) defined as the time from diagnosis to transformation to acute myeloid leukemia.
Results
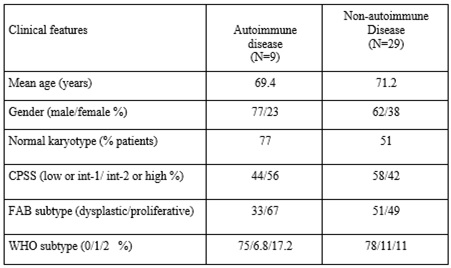
We found a prevalence of AD of 23.6%, with the following autoimmune conditions: primary immune thrombocytopenia (22.2%), psoriasis (22.2%), adult-onset Still’s disease (11.1%), giant cell arteritis (11.1%), ankylosing spondylitis (11.1%), rheumatic polymyalgia (11.1%) and unspecified arthropathy (11.1%). The main clinical features for both groups are described in table 1. The mean follow-up was 32.5 months. PFS at 2 years was 76.5% versus 47.2% in the AD group compared to non-AD group (p: 0.536), respectively.
Conclusion
The patients with CMML and AD represent a special subgroup that could have a better prognosis, as occur in other hematological malignancies. This group of AD tend to have a normal karyotype and dysplastic subtype. More studies could be necessary to confirm the features and clinical evolution of this association.
Session topic: 10. Myelodysplastic syndromes – Clinical
Keyword(s): Autoimmune disease, Chronic myelomonocytic leukemia
Abstract: PB2096
Type: Publication Only
Background
Multiple autoimmune conditions have been described in the context of chronic myelomonocytic leukemia (CMML), but it is not clear if they could have an impact on clinical evolution.
Aims
We describe the subgroup of CMML related to autoimmune diseases (AD) and the main clinical features, compared to the patients who have other types of CMML.
Methods
We have studied 38 patients over 14 years (2003-2016), and compared the subgroup with autoimmune versus non-autoimmune disorders, in order to establish differences in some clinical parameters and the free progression survival (PFS) defined as the time from diagnosis to transformation to acute myeloid leukemia.
Results
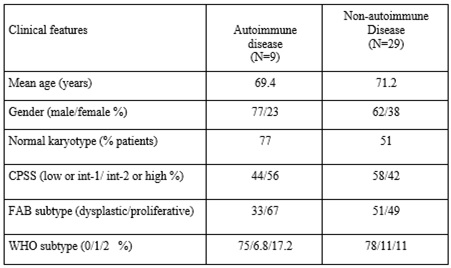
We found a prevalence of AD of 23.6%, with the following autoimmune conditions: primary immune thrombocytopenia (22.2%), psoriasis (22.2%), adult-onset Still’s disease (11.1%), giant cell arteritis (11.1%), ankylosing spondylitis (11.1%), rheumatic polymyalgia (11.1%) and unspecified arthropathy (11.1%). The main clinical features for both groups are described in table 1. The mean follow-up was 32.5 months. PFS at 2 years was 76.5% versus 47.2% in the AD group compared to non-AD group (p: 0.536), respectively.
Conclusion
The patients with CMML and AD represent a special subgroup that could have a better prognosis, as occur in other hematological malignancies. This group of AD tend to have a normal karyotype and dysplastic subtype. More studies could be necessary to confirm the features and clinical evolution of this association.
Session topic: 10. Myelodysplastic syndromes – Clinical
Keyword(s): Autoimmune disease, Chronic myelomonocytic leukemia


