
Contributions
Abstract: PB1897
Type: Publication Only
Background
BCR-ABL tyrosine kinase inhibitors (TKIs) are selective therapies for patients with chronic myeloid leukemia (CML) and induce deep molecular response (DMR). However, many clinical trials of discontinuing TKIs have reported that sustained treatment-free remission (TFR) could only be observed in about 40% of patients for two years. Failure to discontinuation results from the inability of TKIs to eradicate CML leukemia stem cells (CML-LSCs). Among the several factors predict relapse after discontinuation of TKI therapy, only the duration of TKI therapy and DMR closely related to which generation of TKIs was used have been associated with TFR. Furthermore, in our previous observation, 12/22 patients maintained a stable DMR after TKIs withdrawal, and we found patients with second generation TKIs relapsed less than those with Imatinib. Thus we suppose second generation TKIs and Imatinib may have different effects on chronic myeloid leukemia stem cells and affect the outcome of TKIs discontinuation.
Aims
The aim of this study is to investigate how different TKIs affect CML-LSCs in the study of TKIs discontinuation.
Methods
Fresh bone marrow samples were obtained from patients with newly diagnosed chronic phase CML and isolated for CD34+ cells by magnetic cell sorting. Then treated CD34+ cells cultured in growth factors supplemented serum-free medium with Imatinib and Dasatinib for continually three days and stopped for one day. Colony-forming cell (CFC) assays, apoptosis measurement by Annexin-V staining, and cell proliferation detected by WST were performed. Also the three groups of samples were performed proteomic analysis.
Results
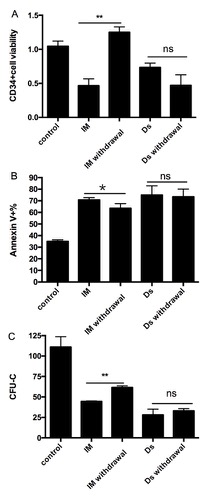
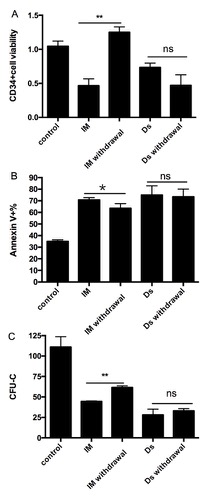
After treating CML CD34+ cells with Imatinib and Dasatinib for 72h, then stopped for 24h, the number of CFU in dasatinib group was less than imatinib group, as proliferation. On the contrary, there was much apoptosis in dasatinib group. Proteomic analysis identified 160 upregulated and 151 downregulated proteins differentially expressed between imatinib group and dasatinib group, which marked enriched in mitochondrial oxidative phosphorylation, including NADH dehydrogenase, cytochrome c oxidase and ATP synthase.
Conclusion
We demonstrated that Imatinib and Dasatinib have obviously different effects on CML-LSCs through regulating metabolism process, specifically promoting oxidative phosphorylation to increase proliferation and avoid apoptosis, which may provide new target for eliminating CML-LSCs in the study of successful TKIs discontinuation.
Session topic: 7. Chronic myeloid leukemia – Biology & Translational Research
Keyword(s): Chronic myeloid leukemia, Mitochondria, Stem cell, Tyrosine kinase inhibitor
Abstract: PB1897
Type: Publication Only
Background
BCR-ABL tyrosine kinase inhibitors (TKIs) are selective therapies for patients with chronic myeloid leukemia (CML) and induce deep molecular response (DMR). However, many clinical trials of discontinuing TKIs have reported that sustained treatment-free remission (TFR) could only be observed in about 40% of patients for two years. Failure to discontinuation results from the inability of TKIs to eradicate CML leukemia stem cells (CML-LSCs). Among the several factors predict relapse after discontinuation of TKI therapy, only the duration of TKI therapy and DMR closely related to which generation of TKIs was used have been associated with TFR. Furthermore, in our previous observation, 12/22 patients maintained a stable DMR after TKIs withdrawal, and we found patients with second generation TKIs relapsed less than those with Imatinib. Thus we suppose second generation TKIs and Imatinib may have different effects on chronic myeloid leukemia stem cells and affect the outcome of TKIs discontinuation.
Aims
The aim of this study is to investigate how different TKIs affect CML-LSCs in the study of TKIs discontinuation.
Methods
Fresh bone marrow samples were obtained from patients with newly diagnosed chronic phase CML and isolated for CD34+ cells by magnetic cell sorting. Then treated CD34+ cells cultured in growth factors supplemented serum-free medium with Imatinib and Dasatinib for continually three days and stopped for one day. Colony-forming cell (CFC) assays, apoptosis measurement by Annexin-V staining, and cell proliferation detected by WST were performed. Also the three groups of samples were performed proteomic analysis.
Results
After treating CML CD34+ cells with Imatinib and Dasatinib for 72h, then stopped for 24h, the number of CFU in dasatinib group was less than imatinib group, as proliferation. On the contrary, there was much apoptosis in dasatinib group. Proteomic analysis identified 160 upregulated and 151 downregulated proteins differentially expressed between imatinib group and dasatinib group, which marked enriched in mitochondrial oxidative phosphorylation, including NADH dehydrogenase, cytochrome c oxidase and ATP synthase.
Conclusion
We demonstrated that Imatinib and Dasatinib have obviously different effects on CML-LSCs through regulating metabolism process, specifically promoting oxidative phosphorylation to increase proliferation and avoid apoptosis, which may provide new target for eliminating CML-LSCs in the study of successful TKIs discontinuation.
Session topic: 7. Chronic myeloid leukemia – Biology & Translational Research
Keyword(s): Chronic myeloid leukemia, Mitochondria, Stem cell, Tyrosine kinase inhibitor


