
Contributions
Abstract: PB1872
Type: Publication Only
Background
Minimal residual disease (MRD) is a powerful prognostic factor in the course of chronic lymphocytic leukemia (CLL). The achievement of MRD negative (MRDneg) remissions is associated with a longer survival of patients with CLL. In addition, it is known that increasing of intensity the induction chemotherapy regimens allows to achieve the maximum eradication of the tumor clone and, thereby, to increase the duration of progression free survival (PFS).
Aims
To assess influence of intensity the induction chemotherapy on the frequency of achievement MRDneg status and duration of PFS.
Methods
In this study were included 118 patients with CLL (male/female ratio 1.3:1), age 31 to 80 years (median 61 years). The median of follow-up duration is 36 months (range 5-84). We have used the revised NCI guidelines (Hallek M, et al., 2008) for diagnosis, initiation of therapy, evaluation of response and MRD (10-4). Patients were treated with rituximab-containing chemotherapy regimens (RFC, RB, RChl, R-CHOP). Median of chemotherapy lines – 1 (range 1-3). Patients were divided into three groups depending on the number of cycles of chemotherapy: group 1 – 4 cycles (n=18), group 2 – 6 cycles (n=78), group 3 – 8 cycles (n=22). The evaluation of MRD status was carried out using 5-color flow cytometry on bone marrow samples after 2 months of completion chemotherapy. In addition, intermediate evaluation of MRD status after 4 treatment cycles was carried out in group 2 (n=36) and group 3 (n=6) underwent.
Results
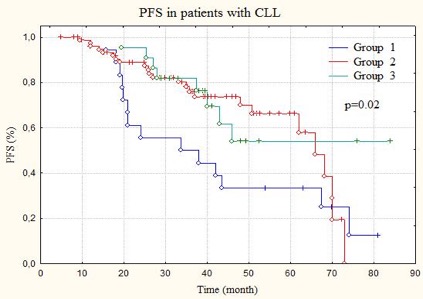
Group 1: complete remission (CR) – 4 (MRDneg – 2), partial remission (PR) – 14 (MRDneg– 2); group 2: CR – 16 (MRDneg – 6), PR – 62 (MRDneg – 26); group 3: CR – 6 (all MRDneg), PR – 16 (none MRDneg). The frequency of achievement of MRDneg status at the completion of chemotherapy regimen was: group 1 – 22.2% (4/18), group 2 – 41.0% (32/78), group 3 – 27.3% (6/22) (p>0.05). The frequency of achievement of MRDneg status after 4 cycles of chemotherapy in group 2 – 22.2% (8/36) and in group 3 – 33.3% (2/6). Median PFS in group 1 was 33.7 months, in group 2 – 66.0 months, and in group 3 – not achieved (p=0.02). When comparing PFS in patients among all groups who achieved MRDneg status after 4 cycles of chemotherapy no significant differences were found, which is probably due to a small number of events and short observation period. However, it was noted that progression/relapse of the disease was occurred only in the group 1 – 11.1% (2/18), while in groups 2 and 3, progression/relapse of the disease was not detected in any patient who achieved MRDneg status after 4 cycles of treatment (p=0.016).
Conclusion
Consider that intensity of chemotherapy does not affect on the frequency of achievement MRDneg status, but affects on PFS, we can assume that patients with a large number of cycles of chemotherapy achieved a deeper MRDneg status (less than 10-4). Intensification of chemotherapy regimens can increase the risk of significant hematologic toxicity and infectious complications, that requires a personified management strategy for patients with CLL.
Session topic: 6. Chronic lymphocytic leukemia and related disorders - Clinical
Keyword(s): chemotherapy, Chronic Lymphocytic Leukemia, Minimal residual disease (MRD), Survival
Abstract: PB1872
Type: Publication Only
Background
Minimal residual disease (MRD) is a powerful prognostic factor in the course of chronic lymphocytic leukemia (CLL). The achievement of MRD negative (MRDneg) remissions is associated with a longer survival of patients with CLL. In addition, it is known that increasing of intensity the induction chemotherapy regimens allows to achieve the maximum eradication of the tumor clone and, thereby, to increase the duration of progression free survival (PFS).
Aims
To assess influence of intensity the induction chemotherapy on the frequency of achievement MRDneg status and duration of PFS.
Methods
In this study were included 118 patients with CLL (male/female ratio 1.3:1), age 31 to 80 years (median 61 years). The median of follow-up duration is 36 months (range 5-84). We have used the revised NCI guidelines (Hallek M, et al., 2008) for diagnosis, initiation of therapy, evaluation of response and MRD (10-4). Patients were treated with rituximab-containing chemotherapy regimens (RFC, RB, RChl, R-CHOP). Median of chemotherapy lines – 1 (range 1-3). Patients were divided into three groups depending on the number of cycles of chemotherapy: group 1 – 4 cycles (n=18), group 2 – 6 cycles (n=78), group 3 – 8 cycles (n=22). The evaluation of MRD status was carried out using 5-color flow cytometry on bone marrow samples after 2 months of completion chemotherapy. In addition, intermediate evaluation of MRD status after 4 treatment cycles was carried out in group 2 (n=36) and group 3 (n=6) underwent.
Results
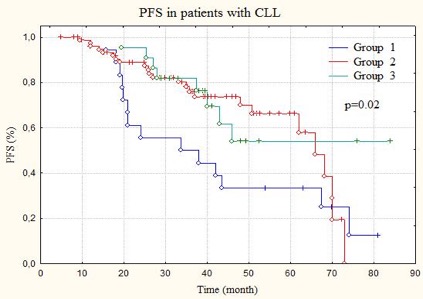
Group 1: complete remission (CR) – 4 (MRDneg – 2), partial remission (PR) – 14 (MRDneg– 2); group 2: CR – 16 (MRDneg – 6), PR – 62 (MRDneg – 26); group 3: CR – 6 (all MRDneg), PR – 16 (none MRDneg). The frequency of achievement of MRDneg status at the completion of chemotherapy regimen was: group 1 – 22.2% (4/18), group 2 – 41.0% (32/78), group 3 – 27.3% (6/22) (p>0.05). The frequency of achievement of MRDneg status after 4 cycles of chemotherapy in group 2 – 22.2% (8/36) and in group 3 – 33.3% (2/6). Median PFS in group 1 was 33.7 months, in group 2 – 66.0 months, and in group 3 – not achieved (p=0.02). When comparing PFS in patients among all groups who achieved MRDneg status after 4 cycles of chemotherapy no significant differences were found, which is probably due to a small number of events and short observation period. However, it was noted that progression/relapse of the disease was occurred only in the group 1 – 11.1% (2/18), while in groups 2 and 3, progression/relapse of the disease was not detected in any patient who achieved MRDneg status after 4 cycles of treatment (p=0.016).
Conclusion
Consider that intensity of chemotherapy does not affect on the frequency of achievement MRDneg status, but affects on PFS, we can assume that patients with a large number of cycles of chemotherapy achieved a deeper MRDneg status (less than 10-4). Intensification of chemotherapy regimens can increase the risk of significant hematologic toxicity and infectious complications, that requires a personified management strategy for patients with CLL.
Session topic: 6. Chronic lymphocytic leukemia and related disorders - Clinical
Keyword(s): chemotherapy, Chronic Lymphocytic Leukemia, Minimal residual disease (MRD), Survival


