
Contributions
Abstract: PB1721
Type: Publication Only
Background
As low minimal residual disease (MRD) value at any time point, assessed by multicolor flow cytometry (MFC) correlates with the better outcome in AML patients (pts), it seems very important to evaluate the impact of treatment intensification on MRD level reduction.
Aims
The aim of the study was to compare the MRD clearance after standard and after intensive consolidation cycles in AML patients and to reveal risk factors of the relapse.
Methods
From March 2016 to February 2018, 60 pts with de novo AML (median age 37, 18-60 yy) were treated in the National Research Center for Hematology, Moscow, with 7+3 (Ara-c 200 mg/m2 c.i, 1-7 days, Daunorubicin 60 mg/m2 1-3 days) as the 1st induction cycle. 39 pts in complete remission (CR) after induction completion were included in the MRD study, comparing different consolidation intensity approaches: (A) 26 pts received 3 «7+3» consolidation cycles with anthracyclines alternation (Daunorubicin 60 mg/m2 in 1st cycle, Idarubicin 12 mg/m2 in 2nd cycle and Mitoxantrone 10 mg/m2 in 3rd 1-3 days with Ara-c 100 mg/m2 bid 1-7 days in each cycle); (B) 13 pts received consolidation with 2 FLARIDA courses (Fludarabine 30 mg/m2 1-4 days, Ara-c 1000 mg/m2 1-4 days, Idarubicin 8 mg/m2 1,3 days). The (A) and (B) cohorts were similar by the age and ELN risk groups. Allogeneic HSCT was performed in 19 pts. MRD was measured in the bone marrow after induction and consolidation by 6 color-MFC on FACS Canto II with a standard antibody panel and 4 tubes, including anti-CD34, CD33, CD117, CD45, CD13, CD11b, CD66b, HLA-DR, CD2, CD4, CD7, CD56, CD38, CD14, CD15, CD16, CD19, CD65, CD99 antibodies. Any detectable MRD value was estimated as MRD positivity; sensitivity level was 0.01%.
Results
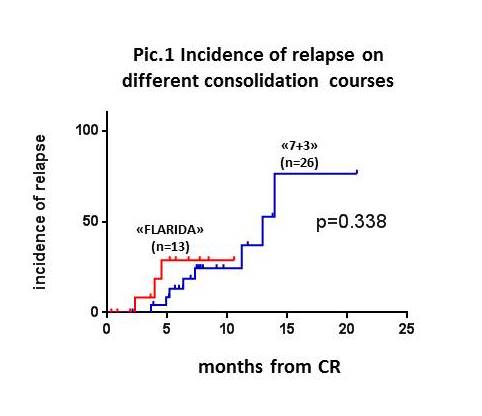
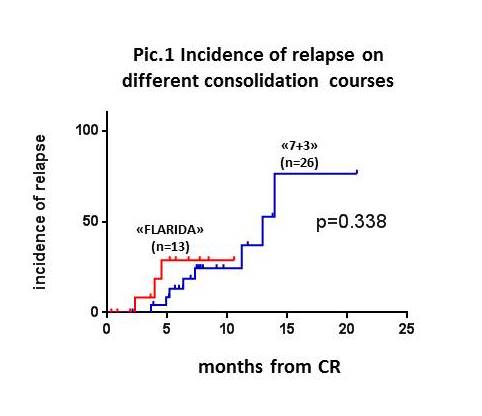
CR after 1st induction 7+3 in the whole cohort was achieved in 41 pts (68%) with MRD-negativity in 27 (65,8%) of them. 26 CR pts after 7+3 consolidation in (A) group have demonstrated much less duration of critical neutropenia (<0,5*109/l) in comparison with 13 CR pts after FLARIDA in (B): 16(1-47) days and 18( 0-35), respectively (p=0,029); median intervals between consolidation courses constituted 32 (30-67) days in (A) vs 38 (29-57) in (B) (p=0,005). The frequency of severe septic complications did not differ in both cohorts: 23.1% (A) vs 46.1%, (B) (p=0,16). MRD-positivity after the 2nd cycle was 3/26 (11,5%) in (A) and 5/13 (38,4%) in (B) cohorts (p=0,08). The same results were obtained after the whole consolidation program - MRD-positivity in 4/21(19%) in (A) and in 2/11 (18%) in the (B) groups (p=0,95). The pts who were MRD-positive after 1st induction had significantly higher relapse risk than MRD-negative: 6/15 (40%) vs 1/27 (3,7%) (p=0,005). Relapse frequency in pts who were MRD-negative after the 2nd course was 26% (6/23) in (A) cohort and 12,5% (1/8) in the (B). The incidence of relapse during 12 months after CR achievement constituted 30,7% in (A) and 23% in (B) cohorts with no significant difference (pic.1).
Conclusion
Though the studied groups are small, we can assume that intensification of consolidation treatment was not translated into better MRD clearance. Moreover, escalation of the chemotherapy induced more profound and prolonged neutropenia with the higher risk of severe infections and more durable intervals between consolidation cycles. The incidence of relapse was comparable in the different by intensity consolidation groups. It’s worth to note that the achievement of MRD negativity after the first induction cycle is associated with better outcome.
Session topic: 4. Acute myeloid leukemia - Clinical
Keyword(s): AML, Chemotherapy toxicity, Minimal residual disease (MRD), Relapse
Abstract: PB1721
Type: Publication Only
Background
As low minimal residual disease (MRD) value at any time point, assessed by multicolor flow cytometry (MFC) correlates with the better outcome in AML patients (pts), it seems very important to evaluate the impact of treatment intensification on MRD level reduction.
Aims
The aim of the study was to compare the MRD clearance after standard and after intensive consolidation cycles in AML patients and to reveal risk factors of the relapse.
Methods
From March 2016 to February 2018, 60 pts with de novo AML (median age 37, 18-60 yy) were treated in the National Research Center for Hematology, Moscow, with 7+3 (Ara-c 200 mg/m2 c.i, 1-7 days, Daunorubicin 60 mg/m2 1-3 days) as the 1st induction cycle. 39 pts in complete remission (CR) after induction completion were included in the MRD study, comparing different consolidation intensity approaches: (A) 26 pts received 3 «7+3» consolidation cycles with anthracyclines alternation (Daunorubicin 60 mg/m2 in 1st cycle, Idarubicin 12 mg/m2 in 2nd cycle and Mitoxantrone 10 mg/m2 in 3rd 1-3 days with Ara-c 100 mg/m2 bid 1-7 days in each cycle); (B) 13 pts received consolidation with 2 FLARIDA courses (Fludarabine 30 mg/m2 1-4 days, Ara-c 1000 mg/m2 1-4 days, Idarubicin 8 mg/m2 1,3 days). The (A) and (B) cohorts were similar by the age and ELN risk groups. Allogeneic HSCT was performed in 19 pts. MRD was measured in the bone marrow after induction and consolidation by 6 color-MFC on FACS Canto II with a standard antibody panel and 4 tubes, including anti-CD34, CD33, CD117, CD45, CD13, CD11b, CD66b, HLA-DR, CD2, CD4, CD7, CD56, CD38, CD14, CD15, CD16, CD19, CD65, CD99 antibodies. Any detectable MRD value was estimated as MRD positivity; sensitivity level was 0.01%.
Results
CR after 1st induction 7+3 in the whole cohort was achieved in 41 pts (68%) with MRD-negativity in 27 (65,8%) of them. 26 CR pts after 7+3 consolidation in (A) group have demonstrated much less duration of critical neutropenia (<0,5*109/l) in comparison with 13 CR pts after FLARIDA in (B): 16(1-47) days and 18( 0-35), respectively (p=0,029); median intervals between consolidation courses constituted 32 (30-67) days in (A) vs 38 (29-57) in (B) (p=0,005). The frequency of severe septic complications did not differ in both cohorts: 23.1% (A) vs 46.1%, (B) (p=0,16). MRD-positivity after the 2nd cycle was 3/26 (11,5%) in (A) and 5/13 (38,4%) in (B) cohorts (p=0,08). The same results were obtained after the whole consolidation program - MRD-positivity in 4/21(19%) in (A) and in 2/11 (18%) in the (B) groups (p=0,95). The pts who were MRD-positive after 1st induction had significantly higher relapse risk than MRD-negative: 6/15 (40%) vs 1/27 (3,7%) (p=0,005). Relapse frequency in pts who were MRD-negative after the 2nd course was 26% (6/23) in (A) cohort and 12,5% (1/8) in the (B). The incidence of relapse during 12 months after CR achievement constituted 30,7% in (A) and 23% in (B) cohorts with no significant difference (pic.1).
Conclusion
Though the studied groups are small, we can assume that intensification of consolidation treatment was not translated into better MRD clearance. Moreover, escalation of the chemotherapy induced more profound and prolonged neutropenia with the higher risk of severe infections and more durable intervals between consolidation cycles. The incidence of relapse was comparable in the different by intensity consolidation groups. It’s worth to note that the achievement of MRD negativity after the first induction cycle is associated with better outcome.
Session topic: 4. Acute myeloid leukemia - Clinical
Keyword(s): AML, Chemotherapy toxicity, Minimal residual disease (MRD), Relapse


