
Contributions
Abstract: PB1737
Type: Publication Only
Background
Treatment of acute myeloid leukemia (AML) is associated with high rate of the life-threating complications requiring intensive care unit (ICU) admission. The long-term outcomes of AML pts discharged from ICU are widely discussable and generally unknown.
Aims
To compare the overall and the disease free survival in de novo AML pts who did not require and those pts who required admission to ICU during remission induction.
Methods
All de novo AML pts, younger than 60 yo, who were treated in NRC from 2013 to 2015 yy, were enrolled into the study evaluating the impact of ICU admission on the long-term outcomes. Median age was – 34 yo (20-60 yo). Patients had advanced disease: LDH activity median 767 u/l (263-5152 u/l); 76% of de novo AML pts had ECOG score 3-4 [1]. Patients were divided into 2 groups: 1st (n=24) – pts who were required ICU admission during induction chemotherapy due to life-threating complications and emergency events and 2nd (n=33) - pts who did not require ICU admission during induction chemotherapy. 3 years overall survival (OS) and disease free survival (DFS) were assessed by the Kaplan – Meier method, log rank value p<0.05 consider as significant. Univariate analysis was performed with χ 2 tests or Fisher’s exact tests for categorical variables to find an independent ICU mortality predictor. All calculations and graphics were performed on IBM SPSS Statistics.
Results
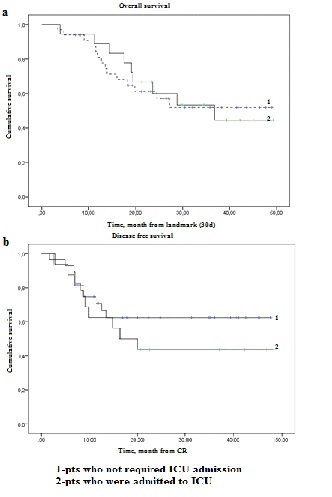
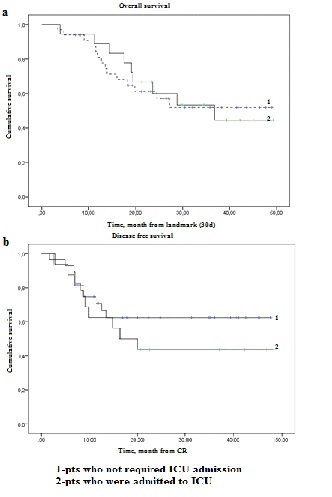
42% (24 of 57 pts) were admitted to the ICU due to life-threating complications and emergency events during induction chemotherapy. All de novo AML pts admitted to ICU were characterized by very advanced disease: LDH activity median 1056 u/l; 25% pts with WBC more than 100 х 109/l; 35% pts of adverse cytogenetic group, - in comparison with pts who did not require admission to ICU: LDH activity median 689 u/l; 15,8% pts with WBC more than 100 х 109/l; 18% pts of adverse cytogenetic risk. Reasons for ICU admissions were the following: acute respiratory failure (ARF) -50 %; acute neurological event – 19,2 %; septic shock (SS) – 11,5 %; urgent caesarian section – 11,5 %; arrhythmia - 7,8 %. ICU survival rate was 75%. 5 pts died due to the SS and 1 due to the ARF. Need for mechanical ventilation, need for vasopressors, 2 and more organ dysfunction were independent significant predictors of ICU mortality (p<0.05). A landmark analysis for OS was performed for patients who survived the first 30 days of treatment (1st induction chemotherapy cycle). OS and DFS were the similar in 1st and 2nd groups; p (log rank) =0.946 and p (log rank) = 0.339 n.s. (picture 1 a, b).
Conclusion
There is no significant difference between 2 groups (ICU requires and non-requires) in OS and DFS. The successfully treated life-threating complications had no influence on the long-term outcomes.
Reference
1. Okhmat V. Paper Poster Session VI Infections in neutropenia and stem cell transplantation Discontinuation of the antibiotic treatment in neutropenic patients with acute myeloid leukaemia ( AML ) / Okhmat V., Korobova A., Parovichnikova E., Troitskaya V., Klyasova G. – 2015. – Т. 5 – С.1208. ECCMID 2015 Copenhagen, Denmark/ https://www.escmid.org/escmid_publications/escmid_elibrary/material/?mid=23676
Session topic: 4. Acute myeloid leukemia - Clinical
Keyword(s): Acute Myeloid Leukemia, Complications, Outcome
Abstract: PB1737
Type: Publication Only
Background
Treatment of acute myeloid leukemia (AML) is associated with high rate of the life-threating complications requiring intensive care unit (ICU) admission. The long-term outcomes of AML pts discharged from ICU are widely discussable and generally unknown.
Aims
To compare the overall and the disease free survival in de novo AML pts who did not require and those pts who required admission to ICU during remission induction.
Methods
All de novo AML pts, younger than 60 yo, who were treated in NRC from 2013 to 2015 yy, were enrolled into the study evaluating the impact of ICU admission on the long-term outcomes. Median age was – 34 yo (20-60 yo). Patients had advanced disease: LDH activity median 767 u/l (263-5152 u/l); 76% of de novo AML pts had ECOG score 3-4 [1]. Patients were divided into 2 groups: 1st (n=24) – pts who were required ICU admission during induction chemotherapy due to life-threating complications and emergency events and 2nd (n=33) - pts who did not require ICU admission during induction chemotherapy. 3 years overall survival (OS) and disease free survival (DFS) were assessed by the Kaplan – Meier method, log rank value p<0.05 consider as significant. Univariate analysis was performed with χ 2 tests or Fisher’s exact tests for categorical variables to find an independent ICU mortality predictor. All calculations and graphics were performed on IBM SPSS Statistics.
Results
42% (24 of 57 pts) were admitted to the ICU due to life-threating complications and emergency events during induction chemotherapy. All de novo AML pts admitted to ICU were characterized by very advanced disease: LDH activity median 1056 u/l; 25% pts with WBC more than 100 х 109/l; 35% pts of adverse cytogenetic group, - in comparison with pts who did not require admission to ICU: LDH activity median 689 u/l; 15,8% pts with WBC more than 100 х 109/l; 18% pts of adverse cytogenetic risk. Reasons for ICU admissions were the following: acute respiratory failure (ARF) -50 %; acute neurological event – 19,2 %; septic shock (SS) – 11,5 %; urgent caesarian section – 11,5 %; arrhythmia - 7,8 %. ICU survival rate was 75%. 5 pts died due to the SS and 1 due to the ARF. Need for mechanical ventilation, need for vasopressors, 2 and more organ dysfunction were independent significant predictors of ICU mortality (p<0.05). A landmark analysis for OS was performed for patients who survived the first 30 days of treatment (1st induction chemotherapy cycle). OS and DFS were the similar in 1st and 2nd groups; p (log rank) =0.946 and p (log rank) = 0.339 n.s. (picture 1 a, b).
Conclusion
There is no significant difference between 2 groups (ICU requires and non-requires) in OS and DFS. The successfully treated life-threating complications had no influence on the long-term outcomes.
Reference
1. Okhmat V. Paper Poster Session VI Infections in neutropenia and stem cell transplantation Discontinuation of the antibiotic treatment in neutropenic patients with acute myeloid leukaemia ( AML ) / Okhmat V., Korobova A., Parovichnikova E., Troitskaya V., Klyasova G. – 2015. – Т. 5 – С.1208. ECCMID 2015 Copenhagen, Denmark/ https://www.escmid.org/escmid_publications/escmid_elibrary/material/?mid=23676
Session topic: 4. Acute myeloid leukemia - Clinical
Keyword(s): Acute Myeloid Leukemia, Complications, Outcome


