
Contributions
Abstract: PB1747
Type: Publication Only
Background
Acute myeloid leukaemia is an oncohaematological disease, with an incidence rate increasing with age. The patients aged above 60 years represent more than 60% of all cases, but the results from the treatment in this age group are worse and the therapeutic approaches available are more limited. With induction mortality rates with standard 7+3 based regimens reaching above 20% in some series one of the most difficult questions in this subset of patients is the proper assessment of the "fitness" of the patients.
Aims
We aimed to assess the therapeutic results from the intensive treatment of AML patients 60 years and older, concerning their overall survival and induction mortality rates and also to identify prognostic factors related to the induction mortality rates in the population of patients which was considered "fit" for intensive 7+3 based induction regimen.
Methods
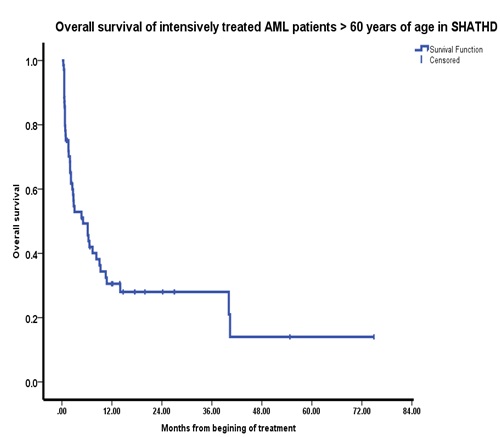
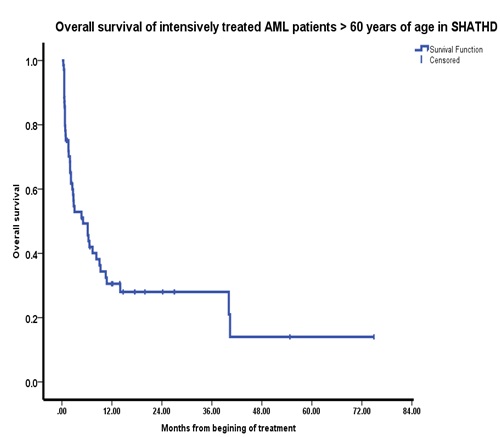
70 patients aged above 60 years with AML, diagnosed and treated intensively for AML in the period from 1.01.2010 to 1.01.2018 were evaluated in the SHATHD (Specialized hospital for active treatment of haematological diseases), with a median of the age of the analysed population of 66 +- 4.08. The treatment consisted of 7+3 based regimens including at least 5 days of administration of Ara-C at a dose above 100 mg per day and at least two administrations of an anthracicline at a standard dose (Epirubicin, Mitoxantron, Idarubicin). We evaluated the overall survival of the patient population, some of the conventional prognostic factors at diagnosis - serum albumin, creatinine, bilirubin, leukocyte count, platelet count, cytogenetic and molecular anomalities, percentage of blast infiltration in marrow, underlining MDS/MPP, some comorbidity indexes (Charlson Comorbidity Index, HCT-CI) and the levels of inductions mortality (IM) rate for the intensively treated patients, defined as mortality within 28 days from the commencing of treatment. The statistical methods used include the methods of Kaplan – Meier, Chi-Square, Fisher’s exact test and Non-parametrical analyses between categorical and continuous variables conducted on the software product SPSS version 22.0
Results
The OS within the study population is 28% at the second year and 14% at he fifth year. The level of the induction mortality as defined above stands at 21.42 %. The analysis of the factors with prognostic significance for induction mortality in patients treated with 7+3 based regimens revealed strongly significant impact of platelet count on induction mortality (p 0.002), pretreatment levels of albumin and creatinine were also significantly affecting prognosis for induction mortality (p 0.028, p.0.030). The lassociation of AML with MDS/MPP also exposed the patients to a significantly higher risk of IM (p. 0.002), while the presence of cytogenetic or molecular aberration correlated with lower risk of IM (p 0.025). Interestingly in our studied population CCI and HCT-CI did not have statistically significant impact on IM.
Conclusion
The increase of the age for intensive treatment of elderly AML patients and the increasing transplant activity in these patients is a global trend now. In order to achieve significantly better results in terms of overall survival, new prognostic systems with a better potential for controlling the treatment related mortality and better selection of the “fitness” of patients for intensive treatment, are needed. This will probably require the development of expected IM risk calculators specific for the elderly patients with AML and their specific risk factors.
Session topic: 4. Acute myeloid leukemia - Clinical
Keyword(s): Acute Myeloid Leukemia, Prognostic factor
Abstract: PB1747
Type: Publication Only
Background
Acute myeloid leukaemia is an oncohaematological disease, with an incidence rate increasing with age. The patients aged above 60 years represent more than 60% of all cases, but the results from the treatment in this age group are worse and the therapeutic approaches available are more limited. With induction mortality rates with standard 7+3 based regimens reaching above 20% in some series one of the most difficult questions in this subset of patients is the proper assessment of the "fitness" of the patients.
Aims
We aimed to assess the therapeutic results from the intensive treatment of AML patients 60 years and older, concerning their overall survival and induction mortality rates and also to identify prognostic factors related to the induction mortality rates in the population of patients which was considered "fit" for intensive 7+3 based induction regimen.
Methods
70 patients aged above 60 years with AML, diagnosed and treated intensively for AML in the period from 1.01.2010 to 1.01.2018 were evaluated in the SHATHD (Specialized hospital for active treatment of haematological diseases), with a median of the age of the analysed population of 66 +- 4.08. The treatment consisted of 7+3 based regimens including at least 5 days of administration of Ara-C at a dose above 100 mg per day and at least two administrations of an anthracicline at a standard dose (Epirubicin, Mitoxantron, Idarubicin). We evaluated the overall survival of the patient population, some of the conventional prognostic factors at diagnosis - serum albumin, creatinine, bilirubin, leukocyte count, platelet count, cytogenetic and molecular anomalities, percentage of blast infiltration in marrow, underlining MDS/MPP, some comorbidity indexes (Charlson Comorbidity Index, HCT-CI) and the levels of inductions mortality (IM) rate for the intensively treated patients, defined as mortality within 28 days from the commencing of treatment. The statistical methods used include the methods of Kaplan – Meier, Chi-Square, Fisher’s exact test and Non-parametrical analyses between categorical and continuous variables conducted on the software product SPSS version 22.0
Results
The OS within the study population is 28% at the second year and 14% at he fifth year. The level of the induction mortality as defined above stands at 21.42 %. The analysis of the factors with prognostic significance for induction mortality in patients treated with 7+3 based regimens revealed strongly significant impact of platelet count on induction mortality (p 0.002), pretreatment levels of albumin and creatinine were also significantly affecting prognosis for induction mortality (p 0.028, p.0.030). The lassociation of AML with MDS/MPP also exposed the patients to a significantly higher risk of IM (p. 0.002), while the presence of cytogenetic or molecular aberration correlated with lower risk of IM (p 0.025). Interestingly in our studied population CCI and HCT-CI did not have statistically significant impact on IM.
Conclusion
The increase of the age for intensive treatment of elderly AML patients and the increasing transplant activity in these patients is a global trend now. In order to achieve significantly better results in terms of overall survival, new prognostic systems with a better potential for controlling the treatment related mortality and better selection of the “fitness” of patients for intensive treatment, are needed. This will probably require the development of expected IM risk calculators specific for the elderly patients with AML and their specific risk factors.
Session topic: 4. Acute myeloid leukemia - Clinical
Keyword(s): Acute Myeloid Leukemia, Prognostic factor


