
Contributions
Abstract: PB1729
Type: Publication Only
Background
Acute Myeloid Leukemia (AML) with NPM mutated (NPM+), FLT3-ITD unmutated (FLT3-) and Normal Karyotype (NK) are included in the favourable cytogenetic-molecular risk class according to the 2010 and 2017 classifications. Frequently, in clinical practice, we focus only on this cytogenetic-molecular risk to define the AML prognosis regardless of clinical risk profile (particularly secondary AML and high blast cells count-BC in peripheral blood-PB, at onset).
Aims
We analyse clinical characteristics, response to chemotherapy (Complete Remission-CR), relapse rate (RR) and outcome of 29 AML NPM+/FLT3-/KN that were homogeneusly treated at our Center in the least 10 years.
Methods
There were 15 female and 14 male with a median age of 53,5 yrs (range 20-68) and 21% of cases had more than 65 yrs. Four (14%) AML were secondary to a previous Myelodysplastic Syndrome and 41% (12/29) had more than 30.000/mmc BC in PB at onset. Overall 52% of case are at High Clinical Risk (HCR) at diagnosis. All patients (pts) were treated with FLAI scheme (Fludarabine, Cytarabin-Ara-C, Idarubicin) as induction, followed by Intermediate dose Ara-C+Idarubicin and High Dose Ara-C, as consolidation therapy.
Results
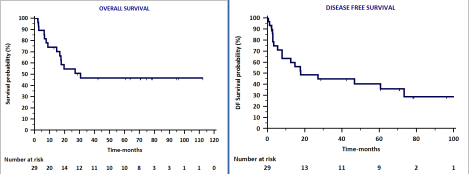
The CR after FLAI was 90% (26/29 cases) and only 7% (2/29) of pts were resistant. DDI was 0%. After a median follow up of 20 months (2-112), 52% of pts (15/29) are alive and 48% (14/29) died. The RR was 41% (12/29) and 8/12 relapsed pts (67%) had CHR at diagnosis. Allo-SCT rate was 41% (12/29) and Allo SCT was performed mainly in CHR and after relapse. The probability of OS at 12, 24 and 36 mths, was 74%, 55% and 47%, respectively (FIGURE 1). The probability of DFS at 12, 24 and 36 mths, was 60%, 48% and 45%, respectively (FIGURE 1). The OS and DFS did not differ between CHR and other pts but we underline that a significant higher proportion of CHR pts received Allo-SCT (10/15 CHR cases vs 2/14 other cases, P<0,05) mainly after their relapse.
Conclusion
In our experience the AML with NPM+/FLT3-/KN have a RR not negligible (41%) with a probability of DFS at 24 mths of 48%. The relapse occured mainly (67%) in pts with CHR (high PB-BC and secondary AML). For this CHR population early and close monitoring of minimal residual disease (quantitative NPM-today available) should be performed in all cases in order to avoid cytologic relapse and to decide if it is worth consolidating their cytologic CR with Allo SCT.
Session topic: 4. Acute myeloid leukemia - Clinical
Keyword(s): Acute Myeloid Leukemia, Flt3-ITD, Risk factor
Abstract: PB1729
Type: Publication Only
Background
Acute Myeloid Leukemia (AML) with NPM mutated (NPM+), FLT3-ITD unmutated (FLT3-) and Normal Karyotype (NK) are included in the favourable cytogenetic-molecular risk class according to the 2010 and 2017 classifications. Frequently, in clinical practice, we focus only on this cytogenetic-molecular risk to define the AML prognosis regardless of clinical risk profile (particularly secondary AML and high blast cells count-BC in peripheral blood-PB, at onset).
Aims
We analyse clinical characteristics, response to chemotherapy (Complete Remission-CR), relapse rate (RR) and outcome of 29 AML NPM+/FLT3-/KN that were homogeneusly treated at our Center in the least 10 years.
Methods
There were 15 female and 14 male with a median age of 53,5 yrs (range 20-68) and 21% of cases had more than 65 yrs. Four (14%) AML were secondary to a previous Myelodysplastic Syndrome and 41% (12/29) had more than 30.000/mmc BC in PB at onset. Overall 52% of case are at High Clinical Risk (HCR) at diagnosis. All patients (pts) were treated with FLAI scheme (Fludarabine, Cytarabin-Ara-C, Idarubicin) as induction, followed by Intermediate dose Ara-C+Idarubicin and High Dose Ara-C, as consolidation therapy.
Results
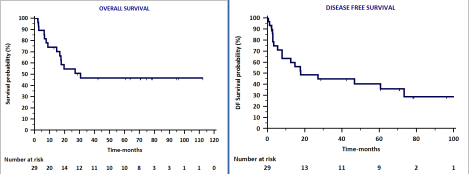
The CR after FLAI was 90% (26/29 cases) and only 7% (2/29) of pts were resistant. DDI was 0%. After a median follow up of 20 months (2-112), 52% of pts (15/29) are alive and 48% (14/29) died. The RR was 41% (12/29) and 8/12 relapsed pts (67%) had CHR at diagnosis. Allo-SCT rate was 41% (12/29) and Allo SCT was performed mainly in CHR and after relapse. The probability of OS at 12, 24 and 36 mths, was 74%, 55% and 47%, respectively (FIGURE 1). The probability of DFS at 12, 24 and 36 mths, was 60%, 48% and 45%, respectively (FIGURE 1). The OS and DFS did not differ between CHR and other pts but we underline that a significant higher proportion of CHR pts received Allo-SCT (10/15 CHR cases vs 2/14 other cases, P<0,05) mainly after their relapse.
Conclusion
In our experience the AML with NPM+/FLT3-/KN have a RR not negligible (41%) with a probability of DFS at 24 mths of 48%. The relapse occured mainly (67%) in pts with CHR (high PB-BC and secondary AML). For this CHR population early and close monitoring of minimal residual disease (quantitative NPM-today available) should be performed in all cases in order to avoid cytologic relapse and to decide if it is worth consolidating their cytologic CR with Allo SCT.
Session topic: 4. Acute myeloid leukemia - Clinical
Keyword(s): Acute Myeloid Leukemia, Flt3-ITD, Risk factor


