
Contributions
Abstract: PB1696
Type: Publication Only
Background
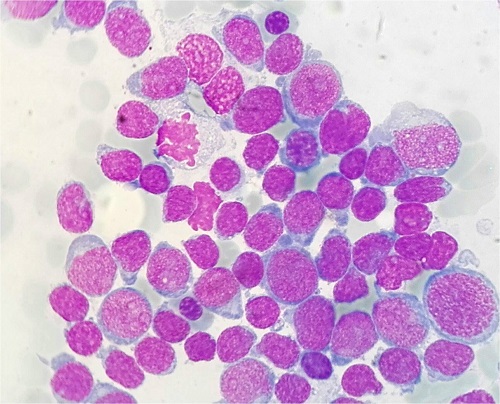
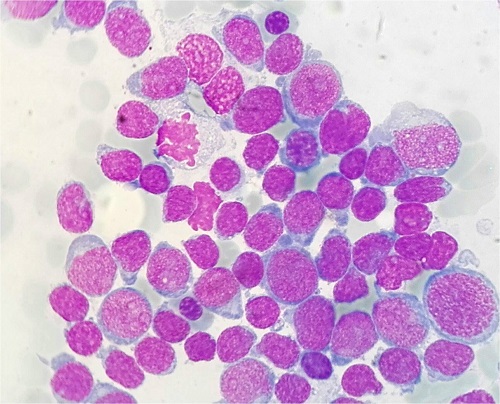
Acute Myeloid Leukaemia with isolated 13 trisomy (AML +13), is classified as intermediate risk-II according with the European Leukaemia Net group (ELN), and has a worse relapse-free and overall survival compared to the other ELN intermediate-II patients, with a median overall survival of 9,3 months. AML +13 has an incidence of 0,7%, it’s associated with undifferentiated morphology and immunophenotype features, and the hand-mirror blast cells are a characteristic finding. Previous works has suggested that AML +13, has a characteristic mutational profile with mutations of RUNX1, SRSF2, ASXL1, BCOR and CEBPZ.
Aims
To describe retrospectively the clinical, biological and morphological data from a cohort of 9 patients diagnosed of AML +13 and compare it with the AML +13 patients from Mehta et al.1 and Harold et al.2 cohorts.
Methods
We collected clinical, morphological and genetic data from 9 patients diagnosed of AML +13 in 5 Catalan hospitals, from September 2013 to May 2017.For the mutational analysis, we used next generation DNA sequencing with a panel of 32 genes often mutates in myeloid malignancies (ABL1,ASXL1,BRAF,CARL,CBL,CEBPA,CSF3R,CSNK1A1,DNMT3A,ETV6,EZH2,FLT3,HRAS,IDH1 IDH2,JAK2,KIT,KRAS,KMT2A,MPL,NPM1,NRAS,PTPN11,RUNX1,SETBP1,SF3B1,SRSF2,TET2,TP53,U2AF1,WT1,ZRSR2). We used MiSeq Ilumina System and SOPHIA DDM software for data analysis.
Results
The most frequently mutated genes in our cohort were RUNX1(7/8, 88%), ASXL1 and SRSF2(4/8, 50%), DNMT3A, FLT3 and TET2(3/8, 38%). Other less frequent mutated genes were IDH2, KMT2A, ZRSR2(2/8, 25%) and EZH2, IDH1, U2AF1, SETBP1, WT1 and CBL(1/8,13%). In Harold et al. cohort, the genes most frequently mutated were SRSF2 81%, RUNX1 75%, ASXL1 44%, BCOR 25%, TET2 19%, IDH2 19% among others, which is comparable with our cohort.In our cohort(n=9) the median age was 72 years-old [58-89], there was a male predominance(8:1), hand-mirror blast cells and small blast cells were present in 89% and 78% of cases, respectively and according FAB classification patients were diagnosed of M0 (n=4), M1(n=4) and M2(n=1), without dysplasia in any case. In the Metha’s cohort(n=23), the median age was 66 years-old, a male predominance(17:6), hand-mirror blast cells and small blast cells were present in 52% and 71% of cases and FAB classification was M0(n=11), M1(n=6), M2(n=2), M4(n=2), M5(n=1), M6(n=1); very similar and comparable with our results.
Three patients were treated with intensive cytarabine-based chemotherapy and one of them underwent allo-transplant, being alive after 6 years from the diagnosis. One patient was treated with hypomethylanting agents, one patient was included in a clinical trial and four patients aged >70 years old received only best supportive treatment. Four patients died due to sepsis (one of them during reinducction after relapse) and four patients died due to haemorrhage. The median overall survival was 8,1 months[0,16-33], being the results comparable with those of other series.
Conclusion
The results of our series were comparable to those described in other series, which supports the different biological and therapeutic behavior from this AML group compared with other AML of the same risk group, according to the ELN.It's possible that the mutational profile, with frequent mutations in the RUNX1, ASXL1, SRSF2, and other genes related to resistance to treatment and less survival, plays a crucial role with the different behavior that AML +13 presents, requiring further studies with larger series to be able to confirm it, and to assess its inclusion as a differentiated entity within the WHO classification.
Session topic: 3. Acute myeloid leukemia - Biology & Translational Research
Keyword(s): Acute Myeloid Leukemia, Cytogenetic abnormalities, Molecular markers, Prognostic factor
Abstract: PB1696
Type: Publication Only
Background
Acute Myeloid Leukaemia with isolated 13 trisomy (AML +13), is classified as intermediate risk-II according with the European Leukaemia Net group (ELN), and has a worse relapse-free and overall survival compared to the other ELN intermediate-II patients, with a median overall survival of 9,3 months. AML +13 has an incidence of 0,7%, it’s associated with undifferentiated morphology and immunophenotype features, and the hand-mirror blast cells are a characteristic finding. Previous works has suggested that AML +13, has a characteristic mutational profile with mutations of RUNX1, SRSF2, ASXL1, BCOR and CEBPZ.
Aims
To describe retrospectively the clinical, biological and morphological data from a cohort of 9 patients diagnosed of AML +13 and compare it with the AML +13 patients from Mehta et al.1 and Harold et al.2 cohorts.
Methods
We collected clinical, morphological and genetic data from 9 patients diagnosed of AML +13 in 5 Catalan hospitals, from September 2013 to May 2017.For the mutational analysis, we used next generation DNA sequencing with a panel of 32 genes often mutates in myeloid malignancies (ABL1,ASXL1,BRAF,CARL,CBL,CEBPA,CSF3R,CSNK1A1,DNMT3A,ETV6,EZH2,FLT3,HRAS,IDH1 IDH2,JAK2,KIT,KRAS,KMT2A,MPL,NPM1,NRAS,PTPN11,RUNX1,SETBP1,SF3B1,SRSF2,TET2,TP53,U2AF1,WT1,ZRSR2). We used MiSeq Ilumina System and SOPHIA DDM software for data analysis.
Results
The most frequently mutated genes in our cohort were RUNX1(7/8, 88%), ASXL1 and SRSF2(4/8, 50%), DNMT3A, FLT3 and TET2(3/8, 38%). Other less frequent mutated genes were IDH2, KMT2A, ZRSR2(2/8, 25%) and EZH2, IDH1, U2AF1, SETBP1, WT1 and CBL(1/8,13%). In Harold et al. cohort, the genes most frequently mutated were SRSF2 81%, RUNX1 75%, ASXL1 44%, BCOR 25%, TET2 19%, IDH2 19% among others, which is comparable with our cohort.In our cohort(n=9) the median age was 72 years-old [58-89], there was a male predominance(8:1), hand-mirror blast cells and small blast cells were present in 89% and 78% of cases, respectively and according FAB classification patients were diagnosed of M0 (n=4), M1(n=4) and M2(n=1), without dysplasia in any case. In the Metha’s cohort(n=23), the median age was 66 years-old, a male predominance(17:6), hand-mirror blast cells and small blast cells were present in 52% and 71% of cases and FAB classification was M0(n=11), M1(n=6), M2(n=2), M4(n=2), M5(n=1), M6(n=1); very similar and comparable with our results.
Three patients were treated with intensive cytarabine-based chemotherapy and one of them underwent allo-transplant, being alive after 6 years from the diagnosis. One patient was treated with hypomethylanting agents, one patient was included in a clinical trial and four patients aged >70 years old received only best supportive treatment. Four patients died due to sepsis (one of them during reinducction after relapse) and four patients died due to haemorrhage. The median overall survival was 8,1 months[0,16-33], being the results comparable with those of other series.
Conclusion
The results of our series were comparable to those described in other series, which supports the different biological and therapeutic behavior from this AML group compared with other AML of the same risk group, according to the ELN.It's possible that the mutational profile, with frequent mutations in the RUNX1, ASXL1, SRSF2, and other genes related to resistance to treatment and less survival, plays a crucial role with the different behavior that AML +13 presents, requiring further studies with larger series to be able to confirm it, and to assess its inclusion as a differentiated entity within the WHO classification.
Session topic: 3. Acute myeloid leukemia - Biology & Translational Research
Keyword(s): Acute Myeloid Leukemia, Cytogenetic abnormalities, Molecular markers, Prognostic factor


