
Contributions
Abstract: PB1704
Type: Publication Only
Background
Mutations that are associated with AML have a high impact on the prognostic of patients, and certain genetic profiles may guide an adequate therapeutic strategy. In Colombia, there are no data on the frequency of mutations associated with this neoplasm.
Aims
To describe the frequency of mutations in a cohort of patients with AML and how they can be related to the response to induction therapy.
Methods
Blood samples were collected from 27 AML patients before and after treatment induction during 2015-2017. Written informed consent was obtained at Hospital Manuel Uribe Angel and Clínica Somer. 500 ng of DNA were used to detect mutations in eight genes related to AML pathogenesis through a customized qBiomarker Somatic Mutation PCR array. For statistics analysis, R v.3.4.3 was used. Patient outcome was modeled using multinomial regression models including molecular and clinical data. Analyses on mutation associations were conducted with logistic regressions. Odds ratio (OR) were determined for regression coefficients and p-values with a Z-Wald test.
Results
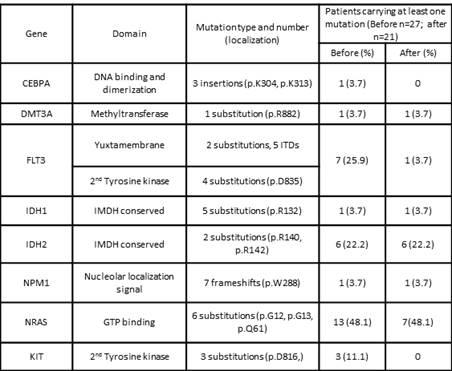
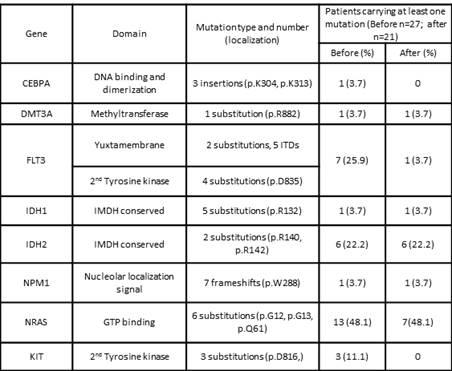
The total number of patients was 27, which were followed for an average of 7 months. Thirteen patients (48,14%) were women and 14 were men (51.85%); age range was 18-78 y (mean 49.9 y). Twenty-one patients survived (77.7%), while 6 died during or after induction treatment (22.3%). Before treatment, the most frequent mutation was NRAS c.35G>A (22.22%), followed by IDH2 c.515G>A (14.81%). After treatment, IDH2 c.515G>A was the most frequent mutation (14.8%), while NRAS c.35G>A corresponded to 11.11%. In 8 patients (29.6%), we found 8 persistent mutations after treatment; curiously all patients (n=4) who had mutation in IDH2 c.515G>A persisted with it after treatment. The logistic regression analysis determined a higher relative risk trend of presenting AML-M1 in patients with FLT3, NRAS or IDH2 mutations. Mutated NRAS and IDH2 after treatment were highly associated with presenting the respective mutation at diagnosis. Multinomial models describing the outcome (death, refractoriness, partial response and complete response) based on molecular and clinical variables suggested -for this cohort of patients-, that mutated FLT3, IDH2 or NRAS after treatment confers a lower OR for death outcome versus complete response. Furthermore, age (OR: 0.56: p = 0.0000025) and blast percentage at diagnosis (OR: 0.69: p = 0.0002645) were inversely associated with complete response compared with patients who died. On the other hand, mutations before treatment in FLT3 were associated with a lower OR in refractoriness or partial response vs. complete response. Finally, mutations in NRAS after treatment had a lower OR in relation to partial response vs. complete response. Results regarding mutations are contradictory to what was previously published, nevertheless, the cohort size and a follow-up of only 7 months could have impacted on results reported here.
Conclusion
We are preliminarily describing the frequency of mutations of a cohort of AML patients in Colombia. Contrary to the literature, we found a high frequency of mutations in IDH2 and NRAS genes, while FLT3 remains as one of the most frequently mutated genes, being FLT3-ITD the most common in our cohort. It is interesting that mutations in IDH2 do not disappear after treatment. In sum, the present work describes gene mutations not previously described in AML Colombian patients. It is necessary to amplify the size of the cohort and to continue the follow-up of patients to observe adverse results that could be correlated with the presence of some mutations.
Session topic: 3. Acute myeloid leukemia - Biology & Translational Research
Keyword(s): Acute Myeloid Leukemia, FLT3, mutation analysis, Ras
Abstract: PB1704
Type: Publication Only
Background
Mutations that are associated with AML have a high impact on the prognostic of patients, and certain genetic profiles may guide an adequate therapeutic strategy. In Colombia, there are no data on the frequency of mutations associated with this neoplasm.
Aims
To describe the frequency of mutations in a cohort of patients with AML and how they can be related to the response to induction therapy.
Methods
Blood samples were collected from 27 AML patients before and after treatment induction during 2015-2017. Written informed consent was obtained at Hospital Manuel Uribe Angel and Clínica Somer. 500 ng of DNA were used to detect mutations in eight genes related to AML pathogenesis through a customized qBiomarker Somatic Mutation PCR array. For statistics analysis, R v.3.4.3 was used. Patient outcome was modeled using multinomial regression models including molecular and clinical data. Analyses on mutation associations were conducted with logistic regressions. Odds ratio (OR) were determined for regression coefficients and p-values with a Z-Wald test.
Results
The total number of patients was 27, which were followed for an average of 7 months. Thirteen patients (48,14%) were women and 14 were men (51.85%); age range was 18-78 y (mean 49.9 y). Twenty-one patients survived (77.7%), while 6 died during or after induction treatment (22.3%). Before treatment, the most frequent mutation was NRAS c.35G>A (22.22%), followed by IDH2 c.515G>A (14.81%). After treatment, IDH2 c.515G>A was the most frequent mutation (14.8%), while NRAS c.35G>A corresponded to 11.11%. In 8 patients (29.6%), we found 8 persistent mutations after treatment; curiously all patients (n=4) who had mutation in IDH2 c.515G>A persisted with it after treatment. The logistic regression analysis determined a higher relative risk trend of presenting AML-M1 in patients with FLT3, NRAS or IDH2 mutations. Mutated NRAS and IDH2 after treatment were highly associated with presenting the respective mutation at diagnosis. Multinomial models describing the outcome (death, refractoriness, partial response and complete response) based on molecular and clinical variables suggested -for this cohort of patients-, that mutated FLT3, IDH2 or NRAS after treatment confers a lower OR for death outcome versus complete response. Furthermore, age (OR: 0.56: p = 0.0000025) and blast percentage at diagnosis (OR: 0.69: p = 0.0002645) were inversely associated with complete response compared with patients who died. On the other hand, mutations before treatment in FLT3 were associated with a lower OR in refractoriness or partial response vs. complete response. Finally, mutations in NRAS after treatment had a lower OR in relation to partial response vs. complete response. Results regarding mutations are contradictory to what was previously published, nevertheless, the cohort size and a follow-up of only 7 months could have impacted on results reported here.
Conclusion
We are preliminarily describing the frequency of mutations of a cohort of AML patients in Colombia. Contrary to the literature, we found a high frequency of mutations in IDH2 and NRAS genes, while FLT3 remains as one of the most frequently mutated genes, being FLT3-ITD the most common in our cohort. It is interesting that mutations in IDH2 do not disappear after treatment. In sum, the present work describes gene mutations not previously described in AML Colombian patients. It is necessary to amplify the size of the cohort and to continue the follow-up of patients to observe adverse results that could be correlated with the presence of some mutations.
Session topic: 3. Acute myeloid leukemia - Biology & Translational Research
Keyword(s): Acute Myeloid Leukemia, FLT3, mutation analysis, Ras


