
Contributions
Abstract: PB1669
Type: Publication Only
Background
Associations between immunophenotypic findings (IF) and genetic abnormalities have been proved for specific subtypes of AML harboring recurrent cytogenetic abnormalities.
Mutation of the nucleophosmin gene (NPM1) is observed in approximately 30% of cases of AML, and is recognized as a distinct entity in the World Health Organization classification. It most commonly falls in the M1/M2 (myeloid) or M4/M5 (myelomonocytic/monocytic) FAB categories and it is associated with a favorable prognosis (although this effect is decreased in the context of concomitant FLT3-ITD mutations).
There is evidence that some cases of NPM1-mutated AMLs are often negative for CD34 and HLA-Dr, showing an acute promyelocytic leukemia-like (APL-like) phenotype although there is limited information about the monocytic pattern of differentiation in these cases.
Aims
To describe the immunophenotypic pattern of the monocytic population in NPM1-mutated AMLs.
Methods
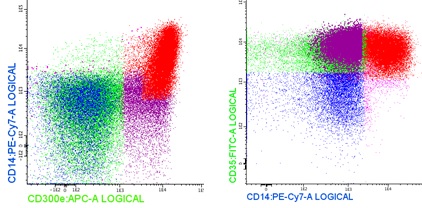
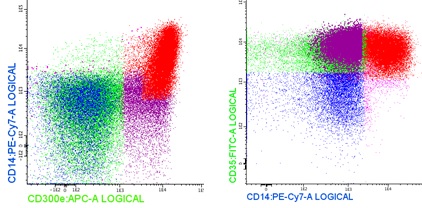
We included BM samples of 9 cases of NPM1-mutated AML (in the absence of the PML-RARA rearrangement). Staining of BM was performed as previously described using the next six-colour combinations of monoclonal antibodies: acute leukemia orientation tubes CD38/CD34/HLA-Dr/CD117/CD19/CD45 and cyMPO/cyCD79α/HLA-Dr/cyCD3/CD34/CD45, monocytic tube CD35/CD64/HLA-Dr/CD14/CD300e/CD45, granulocytic tube CD16/CD13/HLA-Dr/CD10/CD11b/CD45 and erythroid tube CD36/CD105/HLA-Dr/CD117/CD71/CD45. A minimum of 1 million of cells were acquired in a FACSCanto flow cytometer (Becton Dickinson, San Jose, CA, USA) using the FACSDiva software (BD). For data analysis the Infinicyt software (Cytognos, Salamanca, Spain) was used. Monocytic cells were identified by their expression of CD64. As previously described (Matarraz S, et al, 2014) early monocytic cells (CD117low, HLA-Dr++, CD64+, CD14-, CD35- and CD300e-) sequentially acquire reactivity for CD14 and CD35 (promonocytes) and subsequently also for CD300e (mature monocytes). After selecting CD64++ cells (in monocytic cases and also in the residual monocytic cells in the myeloid cases) we identified mature monocytes by their expression of CD300e and in this target population we explored the expression of CD14 and CD35.
Results
The cohort included 5 females and 4 males (F: M ratio = 1.25), with a medium age at diagnosis of 66 years (range 42-87 years). 5 (55 %) cases showed co-mutation of FLT3-ITD. 6 cases (66%) showed morphologic and immunophenotypic evidence of monocytic differentiation, while 3 (33%) of them showed ganulocytic differentiation. All cases were negative for CD34 and 2 were negative for HLA-Dr (22%) showing an “APL-like” phenotype.
All cases studied showed an asynchronous maturation in the monocytic population and the expression of CD300e preceded that of CD14 and/or CD35. The average percentage of the studied population was 4.6%, with a range between 0.3% and 14% (violet population; figure 1).
Conclusion
Our results confirm previous observations regarding the asynchronous maturation in the monocytic population in NPM1-mutated AML (Matarraz S, et al. 2014). These preliminary results must be confirmed in a series with more cases. The expression of CD123, CD25 and CD99 should be included in future studies to explore whether their reactivity associated with the asynchronous pattern here described, can predict the association between NPM1 and FLT3 mutation.
Session topic: 3. Acute myeloid leukemia - Biology & Translational Research
Keyword(s): acute leukemia, Immunophenotype, monocyte
Abstract: PB1669
Type: Publication Only
Background
Associations between immunophenotypic findings (IF) and genetic abnormalities have been proved for specific subtypes of AML harboring recurrent cytogenetic abnormalities.
Mutation of the nucleophosmin gene (NPM1) is observed in approximately 30% of cases of AML, and is recognized as a distinct entity in the World Health Organization classification. It most commonly falls in the M1/M2 (myeloid) or M4/M5 (myelomonocytic/monocytic) FAB categories and it is associated with a favorable prognosis (although this effect is decreased in the context of concomitant FLT3-ITD mutations).
There is evidence that some cases of NPM1-mutated AMLs are often negative for CD34 and HLA-Dr, showing an acute promyelocytic leukemia-like (APL-like) phenotype although there is limited information about the monocytic pattern of differentiation in these cases.
Aims
To describe the immunophenotypic pattern of the monocytic population in NPM1-mutated AMLs.
Methods
We included BM samples of 9 cases of NPM1-mutated AML (in the absence of the PML-RARA rearrangement). Staining of BM was performed as previously described using the next six-colour combinations of monoclonal antibodies: acute leukemia orientation tubes CD38/CD34/HLA-Dr/CD117/CD19/CD45 and cyMPO/cyCD79α/HLA-Dr/cyCD3/CD34/CD45, monocytic tube CD35/CD64/HLA-Dr/CD14/CD300e/CD45, granulocytic tube CD16/CD13/HLA-Dr/CD10/CD11b/CD45 and erythroid tube CD36/CD105/HLA-Dr/CD117/CD71/CD45. A minimum of 1 million of cells were acquired in a FACSCanto flow cytometer (Becton Dickinson, San Jose, CA, USA) using the FACSDiva software (BD). For data analysis the Infinicyt software (Cytognos, Salamanca, Spain) was used. Monocytic cells were identified by their expression of CD64. As previously described (Matarraz S, et al, 2014) early monocytic cells (CD117low, HLA-Dr++, CD64+, CD14-, CD35- and CD300e-) sequentially acquire reactivity for CD14 and CD35 (promonocytes) and subsequently also for CD300e (mature monocytes). After selecting CD64++ cells (in monocytic cases and also in the residual monocytic cells in the myeloid cases) we identified mature monocytes by their expression of CD300e and in this target population we explored the expression of CD14 and CD35.
Results
The cohort included 5 females and 4 males (F: M ratio = 1.25), with a medium age at diagnosis of 66 years (range 42-87 years). 5 (55 %) cases showed co-mutation of FLT3-ITD. 6 cases (66%) showed morphologic and immunophenotypic evidence of monocytic differentiation, while 3 (33%) of them showed ganulocytic differentiation. All cases were negative for CD34 and 2 were negative for HLA-Dr (22%) showing an “APL-like” phenotype.
All cases studied showed an asynchronous maturation in the monocytic population and the expression of CD300e preceded that of CD14 and/or CD35. The average percentage of the studied population was 4.6%, with a range between 0.3% and 14% (violet population; figure 1).
Conclusion
Our results confirm previous observations regarding the asynchronous maturation in the monocytic population in NPM1-mutated AML (Matarraz S, et al. 2014). These preliminary results must be confirmed in a series with more cases. The expression of CD123, CD25 and CD99 should be included in future studies to explore whether their reactivity associated with the asynchronous pattern here described, can predict the association between NPM1 and FLT3 mutation.
Session topic: 3. Acute myeloid leukemia - Biology & Translational Research
Keyword(s): acute leukemia, Immunophenotype, monocyte


