
Contributions
Abstract: PB1633
Type: Publication Only
Background
Acute Lymphoblastic Leukaemia (ALL) is considered rare in elderly patients (pts) but its frequency may be increasing, particularly due to the longer life expectancy of the general population. Management of older pts is an unmet medical need. Significantly lower rates of complete remission, higher early mortality and poorer survival are observed in older compared with younger pts (Gokbuget, 2017). The potential benefit of using moderately intensive chemotherapy protocols for Ph/BCR-ABL-negative ALL and the combination of tyrosine kinase inhibitors (TKI) with chemotherapy in Ph/BCR-ABL positive ALL is debated.
Aims
To analyze the frequency, characteristics and outcome of older pts with ALL consecutively diagnosed at a single Institution receiving treatments of different intensity.
Methods
Of 172 ALL pts diagnosed at our Institution between Jan 2000 to Dec 2017, 38 were > 65 y old (22%). Median age was 73 y (65-88), F/M was 17/19, performance status according to ECOG was 2 in 13 pts and 3 in 14 pts. Molecular analysis, including AF4/MLL and BCR/ABL transcripts (Ph+), were performed in all pts and karyotype was available in 30 (78.9%). According to clinical judgement, age and molecular status pts received intensive treatment (iT) defined as dose-adjusted chemotherapy (da-CT), + TKI in Ph+ (NILG protocols) (Bassan 2015), or non intensive treatment (niT) i.e. steroids, best supportive care (BSC), + TKI alone in Ph+ pts.
Results
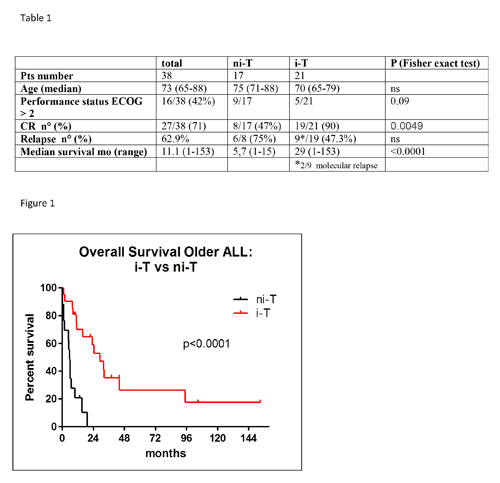
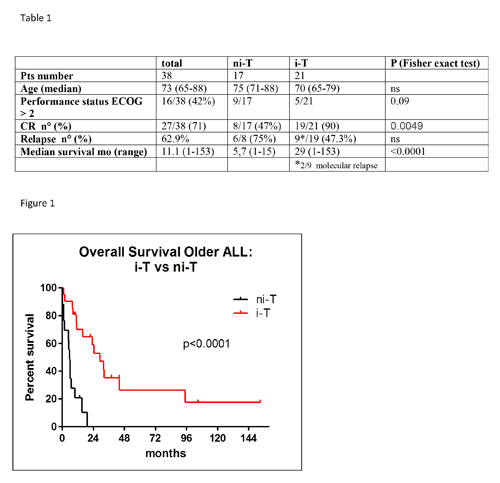
According to the year of diagnosis, the number of elderly ALL pts has increased. Between Jan 2000 and Dec 2008, a lower rate of ALL in pts aged > 65 was observed, compared to the time period Jan 2009-Dec 2017 (6/66, 9% vs 32/106, 30.2%, respectively)(p0.001 chi-squared test). According to phenotype, 32 were B-ALL (84.2%), 1 mixed-phenotype (My-ALL) and 5 (12.8%) were T-ALL/lymphoblastic lymphoma. Two pts showed AF4/MLL rearrangements and 14 were BCR/ABL positive, with e1a2 or b3a2 transcript in 10 and 4 pts, respectively. Karyotype was normal in 7 pts, high hyperdiploidy (He) or near triploidy (Ho-Tr), chromosomal translocations [t(9;22) and t(4;11)] and chromosomal deletions were detected in 4, 16 and 3 pts, respectively. ECOG was >2 in 9/17 niT pts vs 5/21 iT pts (p0.09 Fisher’s exact test). Complete remission and relapse rate were 71% (27/38) and 62.9% (17/27), respectively. Median follow-up of the whole elderly population was 30.5 months (mo) and median survival was 11.1 mo. The main cause of death was disease progression (22/28, 78.6%); other causes were: cardiac (2), myelodysplasia (1), strongyloides infection (1), hepatic failure (1), unknown (1). The characteristics and outcome of iT and niT are summarized in Table 1 and in Figure 1. In particular, median survival of ALL Ph- iT pts was 23,3 mo (1-105 mo) compared to ni-T pts (2 mo, 1-9) (p <0.0001, log-rank test) and median survival of ALL Ph+ iT pts (TKI+da-CT) was 32.4 mo (8-153) compared to ALL Ph+ niT (TKI alone) (6.8 mo, 2-15)(p 0.014 log-rank test). Autologous stem cell transplantation (ASCT) was performed in 7 pts, 4 Ph+ and 3 Ph- (1 MLL/AF4, 1 T-ALL, 1 with HoTr K). Five pts were in molecular CR at the time of ASCT (4 Ph+ and 1 MLL/AF4), two pts were in cytogenetic CR, not available molecular data.
Conclusion
A non-negligible number of pts is diagnosed with ALL over the age of 65, with an incidence that is progressively increasing (27.5% of ALL population). In our experience, intensive treatment including da-CT with TKI in Ph+ pts with or without ASCT was feasible and tolerated, also in a population-based setting, and improved survival both in Ph- but also in Ph+ ALL pts
Session topic: 2. Acute lymphoblastic leukemia - Clinical
Keyword(s): Acute lymphoblastic leukemia, Elderly, epidemiology, Treatment
Abstract: PB1633
Type: Publication Only
Background
Acute Lymphoblastic Leukaemia (ALL) is considered rare in elderly patients (pts) but its frequency may be increasing, particularly due to the longer life expectancy of the general population. Management of older pts is an unmet medical need. Significantly lower rates of complete remission, higher early mortality and poorer survival are observed in older compared with younger pts (Gokbuget, 2017). The potential benefit of using moderately intensive chemotherapy protocols for Ph/BCR-ABL-negative ALL and the combination of tyrosine kinase inhibitors (TKI) with chemotherapy in Ph/BCR-ABL positive ALL is debated.
Aims
To analyze the frequency, characteristics and outcome of older pts with ALL consecutively diagnosed at a single Institution receiving treatments of different intensity.
Methods
Of 172 ALL pts diagnosed at our Institution between Jan 2000 to Dec 2017, 38 were > 65 y old (22%). Median age was 73 y (65-88), F/M was 17/19, performance status according to ECOG was 2 in 13 pts and 3 in 14 pts. Molecular analysis, including AF4/MLL and BCR/ABL transcripts (Ph+), were performed in all pts and karyotype was available in 30 (78.9%). According to clinical judgement, age and molecular status pts received intensive treatment (iT) defined as dose-adjusted chemotherapy (da-CT), + TKI in Ph+ (NILG protocols) (Bassan 2015), or non intensive treatment (niT) i.e. steroids, best supportive care (BSC), + TKI alone in Ph+ pts.
Results
According to the year of diagnosis, the number of elderly ALL pts has increased. Between Jan 2000 and Dec 2008, a lower rate of ALL in pts aged > 65 was observed, compared to the time period Jan 2009-Dec 2017 (6/66, 9% vs 32/106, 30.2%, respectively)(p0.001 chi-squared test). According to phenotype, 32 were B-ALL (84.2%), 1 mixed-phenotype (My-ALL) and 5 (12.8%) were T-ALL/lymphoblastic lymphoma. Two pts showed AF4/MLL rearrangements and 14 were BCR/ABL positive, with e1a2 or b3a2 transcript in 10 and 4 pts, respectively. Karyotype was normal in 7 pts, high hyperdiploidy (He) or near triploidy (Ho-Tr), chromosomal translocations [t(9;22) and t(4;11)] and chromosomal deletions were detected in 4, 16 and 3 pts, respectively. ECOG was >2 in 9/17 niT pts vs 5/21 iT pts (p0.09 Fisher’s exact test). Complete remission and relapse rate were 71% (27/38) and 62.9% (17/27), respectively. Median follow-up of the whole elderly population was 30.5 months (mo) and median survival was 11.1 mo. The main cause of death was disease progression (22/28, 78.6%); other causes were: cardiac (2), myelodysplasia (1), strongyloides infection (1), hepatic failure (1), unknown (1). The characteristics and outcome of iT and niT are summarized in Table 1 and in Figure 1. In particular, median survival of ALL Ph- iT pts was 23,3 mo (1-105 mo) compared to ni-T pts (2 mo, 1-9) (p <0.0001, log-rank test) and median survival of ALL Ph+ iT pts (TKI+da-CT) was 32.4 mo (8-153) compared to ALL Ph+ niT (TKI alone) (6.8 mo, 2-15)(p 0.014 log-rank test). Autologous stem cell transplantation (ASCT) was performed in 7 pts, 4 Ph+ and 3 Ph- (1 MLL/AF4, 1 T-ALL, 1 with HoTr K). Five pts were in molecular CR at the time of ASCT (4 Ph+ and 1 MLL/AF4), two pts were in cytogenetic CR, not available molecular data.
Conclusion
A non-negligible number of pts is diagnosed with ALL over the age of 65, with an incidence that is progressively increasing (27.5% of ALL population). In our experience, intensive treatment including da-CT with TKI in Ph+ pts with or without ASCT was feasible and tolerated, also in a population-based setting, and improved survival both in Ph- but also in Ph+ ALL pts
Session topic: 2. Acute lymphoblastic leukemia - Clinical
Keyword(s): Acute lymphoblastic leukemia, Elderly, epidemiology, Treatment


